The "Iron Triangle" of Minimally Invasive Surgery: Trocars, Staplers, and Ligation Systems
Content
1. The three core instruments of minimally invasive surgery: trocars, staplers, and ligation systems
(1). Trocars: A Key Access Technology for Minimally Invasive Surgery
As modern surgery transitions from traditional open surgery to minimally invasive techniques, trocars, as core instruments for establishing surgical access, play an irreplaceable and fundamental role. This sophisticated medical device opens a "minimally invasive door" to body cavities for surgeons by minimizing tissue trauma, fundamentally changing the concept and practice of surgical access.
In terms of its operating principle, the trocar system utilizes a three-stage process: "puncture-expansion-fixation." Its core structure consists of two main components: a sharp puncture needle and a hollow sheath surrounding it. As the needle penetrates the various layers of the abdominal wall at precisely controlled angles and force, its specially designed beveled tip effectively separates rather than severs muscle fibers. This "blunt dissection" technique significantly minimizes vascular and nerve damage. After puncture, the needle is carefully withdrawn, leaving the sheath as a stable working channel. This channel, typically only 5-12 mm in diameter, can accommodate a variety of surgical instruments, including endoscopic lenses, graspers, and electrocoagulation hooks. Modern, more advanced visualization trocars also integrate micro-cameras and LED lighting systems, enabling real-time image guidance for "what you see is what you insert," minimizing the risk of blind insertion.
In terms of product technical features, contemporary trocar systems demonstrate remarkable engineering innovation. The most notable advancement is the multi-channel integrated design. By integrating three to five independent working channels within a single main sheath, this not only avoids the "Swiss cheese" effect associated with multiple incisions but also significantly improves surgical efficiency. The leak-proof sealing system utilizes a unique silicone valve membrane structure that dynamically maintains stable pneumoperitoneum pressure during instrument insertion and removal, which is crucial for maintaining visual field during laparoscopic surgery. To address the specific needs of different surgeries, trocar diameters range from 3 mm for pediatrics to 15 mm for specialized instrument channels. Of particular note are intelligent trocars with a memory function. The sheath material automatically adjusts its hardness based on changes in body temperature, ensuring the required rigidity during puncture while softening appropriately during indwelling to reduce sustained tissue pressure.

In clinical practice, the value of trocars is reflected in multiple dimensions. During the surgical approach, trocar technology can reduce abdominal wall tissue damage by approximately 70% compared to traditional open incisions, which is crucial for preserving abdominal wall integrity and function. For example, during cholecystectomy, the microchannel created using a trocar reduced postoperative pain scores by over 50% and accelerated the return to walking by two days. During the surgical procedure, the multi-channel trocar system allows the surgical team to achieve true "multi-handed collaboration," allowing the surgeon, assistant, and scope holder to operate their instruments simultaneously without interfering with each other. This enhanced collaborative efficiency has reduced the operating time of complex surgeries, such as radical gastrectomy, by an average of 40%. For applications in specialized populations, such as obese patients, extended trocars address the technical challenges posed by abdominal wall thickness. Their unique tissue expansion design effectively avoids misjudging "false resistance" during puncture.
From a broader perspective, advances in trocar technology have directly driven the development of innovative procedures such as NOTES (Natural Orifice Transluminal Endoscopic Surgery) and single-port laparoscopic surgery. These breakthrough technologies are redefining the boundaries of minimally invasive surgery. Trocars, as fundamental access solutions, remain crucial, offering greater adaptability and innovation within this new surgical paradigm. It is foreseeable that, with the support of intelligent surgical robots and mixed reality navigation systems, trocars will continue to serve as a cornerstone technology for minimally invasive surgery, providing surgeons with safer, more precise, and more convenient surgical access solutions.
(2) Surgical staplers
In the long history of surgical technology development, the invention of staplers transformed traditional manual suturing into a medical device with mechanized precision operation, which not only redefined the technical standards of tissue closure, but also profoundly changed the time dimension and quality dimension of surgical operations. From gastrointestinal anastomosis to vascular reconstruction, from cardiothoracic surgery to gynecological surgery, staplers, with their unique mechanical wisdom and engineering precision, provide surgeons with suturing solutions that exceed the limits of human hands.
The working principle of the stapler embodies the perfect fusion of biomechanics and mechanical engineering. When the surgeon places the tissue to be anastomosed between the jaws of the stapler and pulls the trigger, a series of precise mechanical linkages are immediately deployed. The built-in push plate pushes the pre-loaded suture staples with a constant force. After penetrating the tissue, these specially designed metal staples encounter the resistance of the staple holder and bend into a regular B shape, thereby achieving uniform closure of the tissue. At the same time, the built-in cutting blade moves forward synchronously, completing the neat cutting of the tissue in the center of the suture line, realizing the integrated operation of "suturing-cutting". The entire process is completed in just 0.3 seconds, yet it can achieve uniformity and reliability that are difficult to achieve with manual suturing. Modern electric staplers go a step further. Driven by a micromotor, they digitally control firing force and speed. Combined with a pressure sensor that provides real-time feedback on tissue thickness, they automatically adjust the closing pressure to the optimal range of 30-50 N/cm², avoiding excessive tissue compression or incomplete closure.
From a technical perspective, contemporary stapler systems have evolved into a highly specialized technology platform. Breakthroughs in materials science have enabled staplers to evolve from a single titanium alloy to a wide range of options, including absorbable polylactic acid and nickel-titanium shape memory alloy, to meet the needs of different healing stages. The intelligent stapler design utilizes a color-coded system to intuitively identify the appropriate range of staple leg heights (ranging from 2.0mm to 4.8mm), preventing anastomotic leakage caused by misuse. The introduction of articulating head technology gives staplers 60° of oscillation, enabling multi-angle operation in confined surgical spaces. Even more noteworthy are the new generation of staplers with tissue-sensing capabilities. Through impedance monitoring and thickness measurement, they can automatically identify tissue type and recommend the optimal suturing strategy, significantly lowering the technical barrier for novice surgeons. In specialized surgeries such as sleeve gastrectomy, the three-row staggered staple design provides additional safety, keeping the risk of leakage below 1%.
The role and value of staplers in clinical practice are reflected in multiple aspects. In terms of surgical efficiency, for example, using a stapler for bowel anastomosis during low anterior resection for rectal cancer saves an average of 25 minutes compared to traditional manual suturing, which is of significant significance for long and complex surgeries. Regarding surgical quality, the standardized suturing provided by staplers evenly distributes anastomotic tension, significantly reducing the incidence of postoperative stenosis. Data show that in esophagogastrostomies, mechanical suturing reduces the incidence of anastomotic leakage from 8% with manual suturing to 2.5%. The gentle, uniform compression provided by staplers offers unique advantages for treating delicate tissues such as the lung parenchyma and pancreas, reducing the incidence of air leaks by 60% during lobectomy. In surgeries for obese patients, staplers overcome the technical challenges presented by thick layers of adipose tissue, ensuring reliable closure of full-thickness tissue, a task difficult to achieve with manual suturing.

With the continuous advancement of technology, staplers are becoming increasingly intelligent and precise. The widespread adoption of robotic-assisted surgery has spawned a new generation of intelligent staplers. These devices integrate preoperative CT data to automatically calculate optimal suturing positions and angles. Experimental bio-glue-assisted staplers have begun clinical testing, releasing absorbable bio-glue upon firing to further enhance initial closure strength. Nanotechnology has enabled the surface of suture staples to be loaded with antibiotics or growth factors, achieving dual functions of anti-infection and healing. In the field of remote surgery, 5G-enabled intelligent staplers enable precise procedures under real-time remote expert guidance, bringing benefits to areas with unequal access to medical resources. Advances in stapler technology have not only transformed operating room procedures but have also profoundly impacted overall perioperative management. Standardized mechanical suturing shortens surgical time and reduces anesthesia exposure; reliable anastomosis quality reduces complication rates and shortens hospital stays; and precise tissue processing alleviates postoperative pain and accelerates functional recovery. These combined benefits have made staplers an indispensable technical support for the modern concept of enhanced recovery after surgery (ERAS).
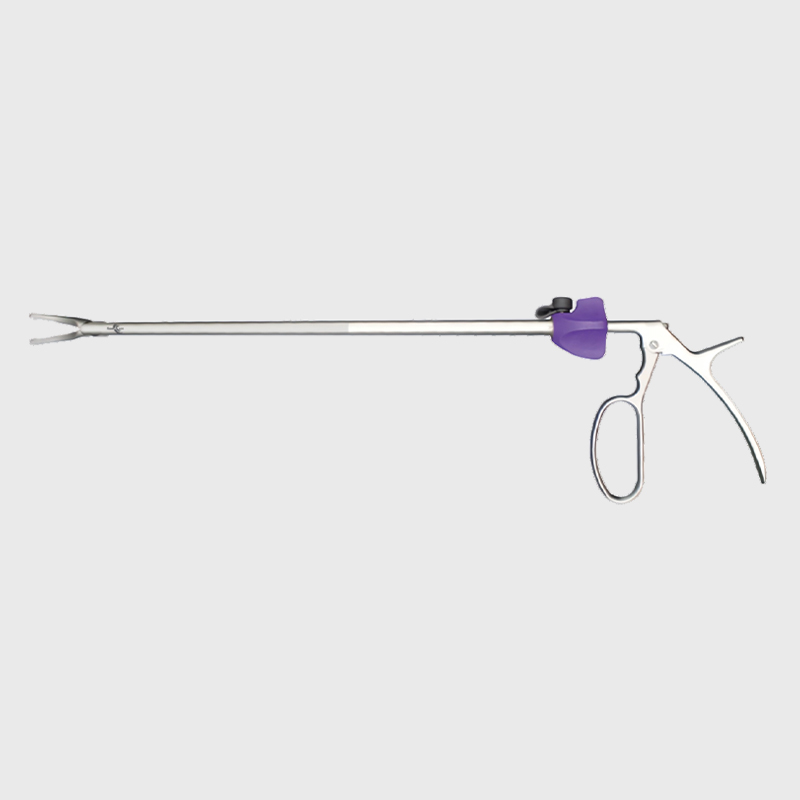
(3) Ligation system: the "safety lock" of vascular management
In surgical operations, vascular ligation technology has always been the key link that determines the success or failure of the operation. From the ancient silk thread ligation to the emergence of modern intelligent ligation systems, this basic operation has undergone a technological transformation. As the core component of minimally invasive surgery, the contemporary ligation system has elevated the basic surgical skill of vascular management to an unprecedented level. In various surgeries such as liver cancer resection, thyroid surgery, and gastrointestinal resection, these sophisticated devices with a metallic luster or transparent polymer materials are reshaping the surgeon's operating experience and the patient's postoperative quality.
The working principle of the ligation system embodies the perfect practice of the multimodal hemostasis concept. The ligation system usually adopts a dual action mechanism of "mechanical compression + energy closure" to achieve permanent occlusion of the blood vessel through the synergy of physical and chemical methods. When the surgeon places the blood vessel between the jaws of the ligation instrument and activates the device, the pre-installed titanium clip or absorbable polymer clip will embrace the blood vessel with constant pressure. Its specially designed tooth structure can generate a holding force of up to 15 Newtons to ensure a close fit to the blood vessel wall. At the same time, the integrated high-frequency electrocoagulation system delivers a precise current of 300-500kHz, denaturing and fusing the collagen in the vessel wall, creating a biological seal in addition to mechanical clipping. This composite ligation technique is particularly suitable for arteries and veins with a diameter of less than 7 mm. Its reliability is particularly outstanding in patients receiving anticoagulation therapy, and the post-operative bleeding rate can be kept below 0.4%. A more advanced ultrasound-activated ligation system further enhances safety by providing real-time feedback on the degree of vessel closure, thereby avoiding tissue carbonization caused by excessive electrocoagulation.
In terms of material selection, medical-grade titanium alloy remains the mainstream due to its excellent biocompatibility. However, the use of absorbable materials such as poly(lactic-co-glycolic acid) (PLGA) addresses the artifact issues associated with metal clips during imaging examinations. These smart materials gradually degrade within 60-90 days, ensuring reliable occlusion during the healing period while avoiding permanent foreign body retention. In terms of ergonomics, the rotating clamp head design enables 360° operation, eliminating the limitations of instrument angle when accessing deep and confined vessels. Pre-loaded multi-shot magazine technology reduces clip replacement time to 3 seconds, significantly improving surgical efficiency. Notably, the intelligent ligation system with self-regulating pressure, whose built-in microsensors automatically adjust clamping force based on vessel diameter and wall thickness, has reduced the recurrent laryngeal nerve injury rate from 3.2% with traditional methods to 0.7% in thyroid surgery. The introduction of fluorescent labeling technology addresses the challenge of postoperative imaging tracking. Barium- or iodine-containing contrast media enable surgeons to clearly identify clip position on X-rays or CT scans.
In clinical practice, innovations in ligation systems have brought multi-dimensional improvements to surgical quality. In hepatobiliary surgery, the use of ultrasonic scalpels combined with intelligent ligation systems has reduced average blood loss during liver resection from over 500 ml to less than 150 ml, significantly improving surgical safety. In vascular aneurysm surgery, anti-slip vascular clips overcome the challenges of high-pressure blood flow, resulting in a clip failure rate of less than 0.1%. The use of absorbable ligation systems in breast surgery and lymph node dissection has significantly reduced postoperative foreign body sensation and improved patients' quality of life. The emergence of magnetically controlled ligation systems on robotic surgical platforms addresses the limited freedom of movement of traditional instruments, enabling more precise vascular dissection through remote magnetic field control. Even in emergency trauma surgery, rapid hemostatic ligation devices can achieve emergency control of major vessels within 30 seconds, buying valuable time for rescue efforts.
2. Maintenance points for trocars, staplers and ligature systems
In the Central Sterilization Supply Center (CSSD), trocars, staplers and ligature systems are the core instruments for minimally invasive surgery. Their performance status directly affects surgical safety and patient prognosis. To ensure the long-term and reliable use of these precision instruments, a scientific maintenance management system must be established.
(1) Maintenance points for trocars
1). Daily cleaning and inspection
Puncture needle core: Immediately after each use, use a soft brush to remove tissue residue, focusing on cleaning the bevel of the needle tip to prevent blood from drying and clogging the spray hole. It should be placed separately during ultrasonic cleaning to prevent collisions that cause curling of the blade. Sheath channel: Use a special pipe brush to thoroughly clear the working channel and check whether the silicone sealing valve is damaged (leakage will make it difficult to maintain pneumoperitoneum). Visualization component: The trocar with a camera needs to be gently wiped with an alcohol pad to avoid scratching the optical coating.
2) Functional Testing
Sealing Test: After assembly, inject air and immerse in water to observe for bubbles and ensure airtightness (maintain 15 mmHg pressure for at least 1 minute).
Multi-channel Patency: Insert simulated instruments of different diameters sequentially to test for uniform resistance across each channel.
3) Regular Deep Maintenance
Bearing Lubrication: Disassemble rotating components quarterly and apply medical-grade silicone grease (such as Dow Corning® 360) to prevent the spray arm from sticking.
Material Integrity Inspection: Use a magnifying glass to inspect the sheath surface for cracks, especially stress concentration areas on reusable sheaths.
4) Special Precautions
Disposable Trocars: Reuse is strictly prohibited. Verify the packaging's sterile barrier is intact before use.
Electric Trocars: Clean the battery contacts monthly with anhydrous ethanol to prevent oxidation and unstable power supply.
(2) Maintenance points of staplers
1). Immediate postoperative treatment
Residue removal of staple cartridge: Immediately disassemble the staple cartridge after firing, and use a hook to remove unfired staples or tissue fragments to prevent blood clots from blocking the staple track. Joint head cleaning: Use a high-pressure water gun to rinse the joint gap and blow it dry with an air gun to prevent residual moisture from causing rust on metal parts.
2). Calibration of key components
Closure pressure test: Use pressure-sensitive paper (such as Fuji® Prescale) to detect the jaw pressure distribution every month. If the deviation exceeds 15%, it needs to be returned to the factory for adjustment. Cutting blade sharpness: Regularly use test materials (such as silicone film) to evaluate the cutting smoothness. Replace the blade when the resistance increases significantly.
3). Electric system maintenance
Battery management: Recharge after full discharge (to avoid "memory effect"). The capacity will decay to 80% after a cycle life of about 300 times. Motor maintenance: The manufacturer's engineer will check the carbon brush wear every six months to prevent unstable speed from affecting the suture quality.
4). Storage requirements
Unopened nail magazine: Store in an environment with humidity <60%. Excessive temperature fluctuations will cause the absorbable nail material to hydrolyze.
Device body: Store in a hanging position to avoid heavy pressure to prevent the jaws from deforming and causing incomplete closure.
(3) Maintenance points of ligation system
1). General cleaning specifications
Clamp guide groove cleaning: Use a fine steel wire to clear the clamp push track after each use to ensure that there is no blood scab or tissue residue.
Electrocoagulation contact maintenance: Use fine sandpaper (2000 mesh) to lightly grind the oxide layer to maintain current conduction efficiency.
2). Functional verification
Clamping force test: Use a standard tensiometer to measure the clamp holding force every week. The titanium clamp should maintain a closing force of ≥10N for 72 hours.
Insulation performance test: For ligation forceps with electrocoagulation function, the insulation resistance of the handle should be tested with a megohmmeter (>100MΩ).
3) Special Maintenance for Absorbable Clips
Humidity Control: Unused PLGA clips should be stored in a desiccating box (containing silica gel desiccant). Moisture absorption accelerates degradation.
Expiration Date Management: Strictly adhere to the "first in, first out" principle. Expired clips may cause incomplete closure.
4) Precision Component Protection
Pressure Sensor: Avoid contact with hard objects in the sensing area. Calibrate within 6 months.
Rotating Mechanism: Apply a small amount of instrument lubricant (such as Triflow®) monthly to maintain smooth 360° rotation.
General Maintenance Principles
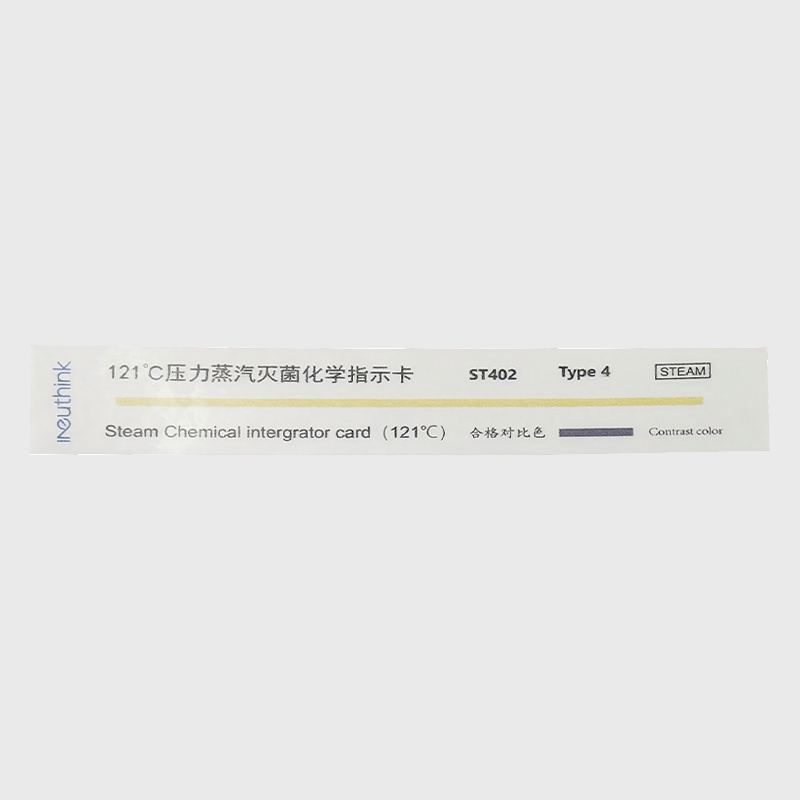
Sterilization Compatibility:
Trocars are autoclavable (sterilization at 134°C), but the motorized components of staplers are only suitable for low-temperature sterilization with ethylene oxide or hydrogen peroxide.
Damage Warning Criteria:
Immediately discontinue use if a scratch depth >0.1mm or joint looseness >0.5mm is detected on the device surface.
Document Traceability Requirements:
Record the device serial number, maintenance details, and test data for each maintenance session and retain them for at least 5 years.
Comparison table of maintenance points for trocars, staplers, and ligation systems:
| Maintenance Items | Trocar | Stapler | Ligation System |
| Daily Cleaning | - Needle core: Remove residue with a soft brush and ultrasonically clean to prevent collisions. | - Remove the staple cartridge to remove residual tissue. | - Clear the clamp push track with a wire. |
| - Sheath: Clear the channel with a dedicated channel brush. | - Flush the joint gap with a high-pressure water jet. | - Polish the electrocoagulation contacts with fine sandpaper. | |
| - Optical lens: Wipe with an alcohol pad. | - Dry with an air gun. | - Clean the rotating mechanism. | |
| Functional Testing | - Airtightness test (15 mmHg for 1 minute) | - Closure pressure test (pressure-sensitive paper) | - Clamping force test (≥10 N for 72 hours) |
| - Multi-channel patency test | - Cutting blade sharpness assessment (silicone membrane test) | - Insulation test (resistance >100 MΩ) | |
| Lubrication and Maintenance | - Apply medical silicone grease to bearings quarterly. | - Apply lubricant to joints monthly. | - Apply a small amount of lubricant to rotating mechanisms monthly. |
| -Prevent seizure of rotating parts. | - Inspect carbon brushes of motor components (six months). | - Protect pressure sensors from contact. | |
| Material Inspection | - Magnifying glass inspection for sheath cracks | - Jaw deformation inspection (disable if gap >0.5mm) | - Titanium clip tooth integrity |
| - Sealing valve integrity test | - Cartridge track wear assessment | - Absorbable clip humidity control (humidity <60%) | |
| Sterilization Management | - High temperature and autoclavable (134°C) | - Electrical components should only be sterilized at low temperatures (EO/H₂O₂) | - Titanium clips can be sterilized at high temperatures |
| - Optical components should be kept away from corrosive disinfectants | - Cartridges should be packaged and sterilized separately | - Absorbable clips should be kept away from high temperatures (<60°C) | |
| Storage Requirements | - Sheaths should be hung vertically to prevent deformation | - Store the electrical components away from moisture | - Absorbable clips should be stored in a desiccant |
| - Disposable trocars should not be reused | - Maintain a constant temperature (20-25°C) and away from light | - Store live devices with power disconnected |
General Maintenance Principles
Damage Standard: Immediately discontinue use if surface scratches >0.1mm or malfunction occurs.
Document Tracking: Record serial number, maintenance details, and test data for ≥5 years.
Personnel Training: Operators must pass a specialized maintenance assessment.
3.What are the common faults of trocars, staplers and ligation systems?
(1) Troubleshooting and Solutions for Trocar Needles
As a crucial instrument for establishing surgical access, trocar needle malfunctions can directly impact the surgical procedure. The most common problem is blockage of the needle lumen, usually caused by tissue debris or clots, resulting in increased resistance during insertion or difficulty in fluid flow. In such cases, immediately cease use, gently clear the blockage with a 0.4mm guidewire, and check for any damage to the needle tip. A more serious issue is sheath seal failure, leading to difficulty maintaining pneumoperitoneum and an unstable surgical view. This often occurs due to aging of the silicone seal or damage from repeated punctures. A leak test with air and water can pinpoint the leak location. Minor damage can be temporarily repaired with medical-grade silicone, but severe damage requires replacement of the entire sealing component.
Malfunctions of the imaging system in visual trocar needles are also significant. Common problems include lens fogging, blurry images, or abnormal illumination. These are usually caused by improper lens cleaning or LED light source degradation. Use specialized lens cleaning paper and anhydrous ethanol; avoid using ordinary gauze. For illumination issues, check the fiber optic connection; replace the light source module if necessary. Motor drive malfunctions in motorized trocar needles manifest as inconsistent or intermittent insertion force, often due to oxidized battery contacts or worn motor brushes. Regularly clean the contacts with electronic cleaner and perform professional motor maintenance every six months.
(2) Analysis of common malfunctions of staplers
Stapler malfunctions may lead to serious intraoperative complications. The most dangerous malfunction is incomplete firing, which is manifested as some staples in the staple cartridge failing to form properly. This is usually caused by the staple pusher being stuck or the tissue being too thick and exceeding the instrument load. Once this happens, do not force a second firing, and keep at least a 2mm safety margin to reload the staple cartridge. Poor staple forming is another common problem, which is manifested as irregular curvature or inconsistent leg length of the B-shaped staple. This is mostly caused by wear of the staple holder or instrument calibration deviation. The forming quality needs to be verified by testing materials. If the deviation exceeds 15%, professional calibration is required.
The electronic system failure of electric staplers is particularly complex. Sudden battery power failure may cause firing interruption. In this case, a manual emergency release device should be available. More insidious is pressure sensor drift, which will cause abnormal closing pressure and increase the risk of tissue damage. It is recommended to calibrate with a standard pressure tester every month. If the error exceeds 10%, it needs to be returned to the factory for repair. Joint head loosening is a typical mechanical failure after long-term use, which is manifested by a swing gap of more than 0.5mm between the jaws, which will seriously affect the suturing accuracy. The rotating bearing assembly must be replaced in time.
(3) Failure Modes and Troubleshooting of the Ligation System
The reliability of the ligation system directly affects hemostasis during surgery. Incomplete clamping is the most common mechanical failure, manifested as the vascular clamp failing to completely occlude the vessel. This is usually due to wear of the clamp's pushing mechanism or the vessel diameter exceeding the device's nominal range. The solution is to immediately add another hemostatic clamp proximally and check for any tissue debris in the clamp's groove. More dangerous is clamp detachment, which often occurs when handling high-pressure vessels. This is related to design flaws in the anti-slip mechanism or improper operating angle. Selecting a vascular clamp with bidirectional anti-slip serrations can reduce this risk.
Failure of the electrocoagulation function is a major problem with combined ligation systems. It manifests as severe tissue adhesion without effective coagulation, usually caused by oxidation of the electrocoagulation contacts or unstable current output. Regular maintenance of the contacts with conductive grease and verification of circuit integrity using an impedance tester are crucial. Premature degradation of absorbable clamps is a specific failure mode, characterized by a rapid decrease in clamp strength shortly after surgery. This is often related to excessive humidity during storage; strict control of warehouse humidity below 60% and periodic testing of the mechanical properties of the clamps are essential.
(4) Preventive Strategies for Common Failures
The issue of seal failure, common to all three types of devices, requires special attention. Whether it's the loss of airtightness in the cannula needle, the aging of the dust-proof seal in the suture device, or the deterioration of the waterproof performance of the ligation system, all can lead to sterilization agent penetration and internal corrosion. It is recommended to conduct seal performance tests quarterly and use silicone-based lubricants to extend the lifespan of the seals. Another common problem is the decline in precision due to mechanical wear, which necessitates regular performance verification using standard test fixtures and a comprehensive preventive maintenance program.
Electronic system failures in medical devices can range from moisture on circuit boards to program errors. This requires CSSDs to establish dry storage systems and equip critical equipment with backup power supplies. With the application of IoT technology, remote diagnostic systems can provide early warning of 80% of potential failures, making them worthy of adoption in large medical centers. All maintenance operations must include detailed documentation of the device serial number, failure symptoms, and corrective actions. This data not only optimizes maintenance cycles but also provides valuable insights for manufacturers to improve their designs.
Common faults and treatment comparison table of trocars, staplers and ligation systems:
| Fault Type | Fault Symptom | Possible Cause | Emergency Actions | Long-Term Solution |
| trocar | ||||
| Needle core obstruction | Increased puncture resistance, poor flushing fluid flow | Obstruction by tissue debris/blood clots, curled needle tip | Use a 0.4mm clear needle to clear the area and replace with a spare core needle | Immediate postoperative flushing and anti-thrombin pretreatment |
| Sheath seal failure | Unstable pneumoperitoneum pressure, leak alarm | Silicone valve aging, repeated instrument puncture damage | Temporary repair with medical silicone and adjustment of pneumoperitoneum flow rate | Replace the sealing valve every 30 cycles and avoid rough handling |
| stapler | ||||
| Incomplete firing | Partial staple formation, tissue not closed | Stapling plate stuck, tissue too thick | Re-suture with a 2mm safety margin | Assess tissue thickness preoperatively and select an appropriate staple cartridge |
| Poor staple formation | Irregular curvature of B-shaped staples, weak closure | Abutment wear, instrument misalignment | Manually reinforce sutures | Calibrate monthly with test material; return if deviation >15% |
| Ligation system | ||||
| Incomplete clipping | Incomplete closure of the blood vessel, bleeding | Worn push mechanism, oversized blood vessel | Additional hemostatic clip at the proximal end | Select the appropriate clip size and inspect the guide groove for wear monthly |
| Clip detachment | Postoperative rebleeding | Anti-slip design defects, improper operating angle | Emergency secondary surgery for hemostasis | Use bidirectional non-slip serrated clips and provide training on standardized operating angles |
Supplementary Fault Management Instructions
Priority Action: Failures affecting patient safety (e.g., stapler firing failure, ligation clip detachment) require immediate termination of surgery and activation of the emergency plan.
Testing Standards:
Trocar Air Tightness Test: Maintain 15 mmHg pressure for 1 minute with no leakage.
Stapler Closure Pressure: Verify uniformity using standard pressure test paper.
Ligation Clip Retention Force: ≥10 N for 72 hours.
Documentation Requirements: Record the faulty device serial number, time of occurrence, personnel involved, and follow-up. Retention period: ≥5 years.
4.FAQs about trocars, staplers, and ligation systems
(1) About the trocar
1). Question: What are the key techniques for puncturing with a trocar?
A: The key lies in stability, accuracy, and gentle handling. First, choose a blood vessel with good elasticity and diameter. Before puncturing, ensure the trocar lumen is filled with fluid (such as saline) and all air is expelled to prevent air embolism. During puncture, quickly insert the needle at an appropriate angle (usually 15-30 degrees). After blood flow is observed, lower the angle and insert it slightly parallel to ensure both the trocar and the needle core are fully inside the blood vessel. Then, secure the needle core, push the trocar completely into the blood vessel, and finally remove the needle core.
2). Question: How to prevent trocar blockage?
A: Prevention of blockage mainly relies on standardized flushing and sealing procedures. During infusion breaks, the line should be regularly flushed with saline or diluted heparin saline. After infusion, use "positive pressure sealing" (clamping the catheter or withdrawing the syringe while injecting the sealing fluid) to prevent blood from flowing back to the trocar tip and forming a clot.
(2) About suturing devices (using vascular suturing devices as an example)
1). Question: How does a vascular suturing device work?
A: It is a device that efficiently closes vascular puncture sites. Its principle mimics a surgeon's suturing technique. When placed in the blood vessel, the device automatically deploys a suture needle, forming a pre-set knot inside and outside the vessel wall. The operator only needs to tighten the knot externally, thus sealing the puncture from the outside and achieving rapid and reliable hemostasis.
2). Question: What are the important precautions when using a vascular suturing device?
A: The precautions are crucial:
Angle and position: When inserting the device, ensure the correct angle with the blood vessel (usually 45 degrees) and confirm the device tip is fully inside the vessel; otherwise, suture failure or vessel damage may occur.
Confirm the "suture anchor": Before tightening the knot, confirm via fluoroscopy or palpation that... The "foot" of the suture must properly engage the blood vessel wall. This is the foundation for successful suturing. Aseptic technique: The entire procedure must strictly adhere to aseptic principles to prevent infection.
(3) About the ligation system
1). Question: What is the difference between simple ligation and suture ligation?
A: These are two different ligation techniques:
Simple ligation: This is the most common method, which involves directly wrapping the suture around the blood vessel or other tubular structure and tying it tightly. It is suitable for most cases.
Suture ligation (also known as "through-and-through ligation"): This is mainly used for important blood vessels or tissue pedicles, or when there is a risk of the blood vessel slipping off. The method involves passing a needle and thread through the center of the blood vessel or tissue, and then wrapping it around the ligature. This provides added security and greatly reduces the risk of the ligature slipping off.
2). Question: What is the most important thing to consider when ligating?
A: The key is "appropriate tension, firm and reliable".
When tying the knot, the tension should be consistent and neither too tight nor too loose. Too tight may damage delicate tissue or break the suture; too loose may cause the ligation to fail and lead to postoperative bleeding. Ensure the knot is a standard surgical knot (such as a square knot) to prevent it from loosening.



 English
English Español
Español Français
Français










 CONTACT US
CONTACT US