What are the uses of disposable medical masks?
Content
- 1 1. What is a Disposable Medical Mask?
- 2 2. Usage Guidelines for Disposable Medical Masks
- 3 3.Storage conditions of disposable medical masks
- 4 4.Guidelines for handling abnormal situations of disposable medical masks
- 5 5. Disposal of disposable medical masks after use
- 6 6.How long can disposable medical masks be used?
- 7
- 8 7.Frequently asked questions about disposable medical masks
- 8.1 (1). What is the difference between disposable medical masks and surgical masks?
- 8.2 (2). How long can disposable medical masks be used? Can they be reused?
- 8.3 (3). Does wearing the mask upside down affect its protection?
- 8.4 (4). Can masks be disinfected with alcohol or UV light?
- 8.5 (5). Can children wear adult masks?
- 8.6 (6). What should I do if I experience skin allergies or acne after wearing a mask?
- 8.7 (7). What is the purpose of the nose clip on a mask? How do you properly shape it?
- 8.8 (8). How should a used mask be disposed of?
- 8.9 (9). Why do glasses fog up when wearing a mask? How can this be fixed?
- 8.10 (10). Do disposable medical masks protect against PM2.5 and viruses?
1. What is a Disposable Medical Mask?
In today's healthcare sector, disposable medical masks have become the first line of defense for protecting both medical staff and the public. This seemingly simple piece of protective equipment is actually a sophisticated device that integrates the wisdom of multiple disciplines, including materials science, microbiology, and ergonomics. From the sterile environment of the operating room to daily disease prevention, from industrial dust control to emergency response to public health emergencies, disposable medical masks, with their unique protective properties and convenient use, play an irreplaceable role worldwide.
The core function of disposable medical masks is to provide an effective respiratory barrier. Their typical three-layer structure forms a complete protective system: an outer layer of water-repellent nonwoven fabric blocks droplets and larger particles; a middle meltblown fabric acts as the core filter layer, capturing small particles and pathogens through electrostatic adsorption; and an inner layer of moisture-absorbing nonwoven fabric ensures wearer comfort. This structural design enables the mask to effectively filter airborne particles ≥3 microns, with a bacterial filtration efficiency (BFE) typically exceeding 95%. In clinical settings, this filtration efficiency can significantly reduce the risk of microbial transmission between medical staff and patients during surgery.
Disposable medical masks, as a crucial component of modern medical protection systems, serve far more than simply providing physical protection. This seemingly simple piece of protective equipment actually delivers comprehensive protection through multiple mechanisms, building an invisible health barrier in both medical practice and public health. At a microscopic level, the mask's multi-layered composite structure forms a sophisticated filtration system. The outer layer of water-repellent nonwoven fabric effectively intercepts droplets and larger particles, the middle meltblown fabric captures tiny particles and pathogens through electrostatic adsorption, and the inner layer's soft material ensures wearer comfort. This design enables the mask to achieve a bacterial and viral interception efficiency of over 95%. In clinical settings, it is not only a key piece of equipment for preventing microbial contamination in the operating room, significantly reducing the rate of surgical site infections, but also an essential safeguard for medical staff against splashes of blood and body fluids during daily consultations. Its protective value is particularly evident during aerosol-generating procedures such as dental treatment and endoscopic examinations. During major infectious disease outbreaks, disposable medical masks demonstrate the
ir unique value in protecting the public. By blocking the droplet transmission chain, they can effectively slow the spread of the epidemic, a fact that has been fully demonstrated in the COVID-19 pandemic prevention and control efforts. Beyond their direct biological protection capabilities, these masks can also filter out allergens like pollen and dust from the air, providing protection for susceptible individuals. In industrial environments, they are essential equipment for combating occupational dust hazards. Notably, the protective effectiveness of masks extends beyond physical protection. Their visual protection features can also have significant social and psychological benefits, enhancing public awareness of self-protection and alleviating public anxiety during these challenging times. Technological advances are empowering modern medical masks with more innovative features, such as smart masks with integrated physiological parameter monitoring sensors and cutting-edge products using biodegradable and environmentally friendly materials, continuously expanding the boundaries of protection. Of course, to fully realize the protective value of masks, they must be worn correctly and replaced frequently, and they must work synergistically with other protective measures to form a comprehensive health protection system. From personal protection to public health, from medical professionals to everyday life, disposable medical masks, with their scientific design and reliable performance, continue to provide a fundamental and vital safeguard for human health.

2. Usage Guidelines for Disposable Medical Masks
In public health and medical practice, disposable medical masks, as essential protective equipment, are highly dependent on standardized usage procedures to maximize their effectiveness. From unpacking and donning to proper disposal after use, each step is based on rigorous scientific evidence and practical key points. Only by systematically mastering these regulatory requirements can we truly establish an effective respiratory protection barrier.
The protective mechanism of disposable medical masks is based on fluid mechanics and materials science. In their three-layer design, the outer layer of water-repellent non-woven fabric blocks droplets through surface tension, the middle meltblown fabric captures particles through electrostatic adsorption, and the inner layer of moisture-absorbing material balances breathability and comfort. This precise construction requires that each functional layer be correctly positioned during use. Any incorrect wearing method can reduce protective effectiveness by over 30%. Research data shows that properly worn medical masks can reduce the risk of respiratory disease transmission by 60-80%, while improper use can reduce protective effectiveness to less than 40%.
Proper use begins with thorough preparation before donning. Operators should choose genuine masks that comply with YY/T 0969 or corresponding national standards and verify the packaging integrity and expiration date. Environmental preparation is also crucial. Hands should be handled in a clean area and should be avoided in areas with high contamination risk. Hand disinfection is an often-overlooked but crucial step. We recommend thorough handwashing using the seven-step handwashing method or using an alcohol-based quick-drying hand sanitizer to ensure the microbial load on hands is reduced to a safe level. Studies have shown that direct contact with the inner layer of a mask without proper hand disinfection increases the risk of contamination by 3-5 times.
The actual wearing process requires precise operation procedures. When unpacking, avoid touching the inside of the mask with your fingers and handle it by the ear straps or headband. When unfolding, distinguish between the inner and outer layers (usually the darker or waterproof surface is on the outside). The upper and lower directions are determined by the position of the nose clip. When fitting, first secure the nose clip to ensure a close fit to the bridge of the nose. Then unfold the mask to cover the mouth, nose, and jaw. Finally, adjust the tightness of the ear straps. It is particularly important to avoid touching the outer surface of a mask with your hands while wearing it. Clinical observations have shown that such improper contact can transfer pathogens from the mask surface to your hands in up to 72%.
Masks require continuous quality monitoring after they are put into use. It is recommended to keep personal records of wearing time. Ordinary medical masks should not be used continuously for more than four hours or should be replaced promptly if humidity increases. If obvious contamination (such as droplet spray), structural damage (such as ear strap breakage), or a significant increase in breathing resistance occurs during use, the mask should be replaced immediately. It is important to emphasize that when temporarily removing a mask, it should not be hung around the neck or placed in a pocket. This improper handling increases the risk of contamination of the mask's inner layer by 80%. The correct approach is to prepare a dedicated sealed bag for temporary storage or replace the mask directly.
In high-risk environments, such as medical settings, mask usage regulations are even stricter. In sterile areas such as operating rooms, masks must fully cover the mouth, nose, and beard, and repositioning during surgery is prohibited. When performing aerosol-generating procedures such as endotracheal intubation and suctioning, choose a mask with higher filtration efficiency (e.g., ASTM Level 2 or higher) and ensure that the edge of the mask seamlessly connects to the face shield. Epidemiological surveys show that in COVID-19 ICU wards, healthcare workers who properly used high-level protective masks had a 67% lower infection rate than those wearing standard masks.
The handling of the mask during removal also affects its overall protective effectiveness. It is recommended to remove it partially by the ear or headband to avoid touching the potentially contaminated outer layer. Hand disinfection should be performed immediately after removal, as this step can reduce the risk of contact transmission by over 60%. Used masks should be disposed of as medical waste in a dedicated collection container or sealed and discarded in ordinary locations. Studies have shown that viruses can survive on the surface of discarded masks for up to 7 days. Standardized disposal procedures are crucial to interrupting the chain of transmission.
There are many misconceptions in practice that require vigilance. Reusing disposable masks is a common misconception. Experimental data shows that masks treated with ethanol spray have a 90% decrease in filtration efficiency. Wearing a double-layer mask, while seemingly enhancing protection, actually compromises the seal and increases leakage by 45%. Wearing the mask with the nose exposed completely negates any protective effect. These misconceptions require systematic health education to address them. Individualized guidance is needed for special populations, such as children and those with respiratory diseases. Children should choose masks specifically sized for their condition, with adjustable ear straps to ensure a snug fit. Parents should supervise and ensure that masks are worn for no more than two hours. Patients with chronic obstructive pulmonary disease can choose modified models with exhalation valves, but be aware that these masks lack bidirectional protection. Individuals with distinctive facial features (such as beards) should opt for headband masks or use sealing strips.
A comprehensive protective system requires an effective verification mechanism. Medical institutions can assess the tightness of masks using fluorescence testing. Ordinary users can use a simple "breath test": quickly exhale over the mask with both hands to feel for leaks around the edges. New smart masks are beginning to integrate sensors to monitor filtration efficiency and wear status in real time. These technological innovations are driving precision in protective measures. During public health emergencies or periods of material shortages, a tiered usage strategy can be implemented. Prioritize the use of high-grade protective masks in high-risk scenarios (such as exposure procedures in medical institutions). For more general protection, extended use can be appropriately extended, but not exceeding eight hours. The key is to establish a scientific risk assessment system that balances resource allocation with protective needs. From individual protection to mass epidemic prevention, the standardized use of disposable medical masks forms a dynamic protective network. This seemingly simple protective action actually integrates the insights of multiple disciplines, including materials science, fluid mechanics, epidemiology, and clinical medicine. As global public health challenges become increasingly complex, only by transforming standardized procedures into muscle memory can we truly unleash the full potential of this fundamental protective technology and provide a solid foundation for building a healthy defense line. Remember: the best mask is one that is worn correctly, and the most effective protection is standardized protection.
Specifications for the use of disposable medical masks
| Steps | Standardized Operations | Prohibited Behaviors | Scientific Basis |
| Preparation Before Wearing | 1. Select a mask that complies with the YY/T 0969 or GB 19083 standards. 2. Check that the packaging is intact and within the expiration date. 3. Thoroughly clean your hands with soap or alcohol-based hand sanitizer (seven-step handwashing method). | 1. Using a mask with damaged packaging or expired. 2. Directly touching the inner layer of the mask without washing hands. | Pathogens carried on hands may contaminate the inner layer of the mask, reducing its protective effectiveness (research shows that wearing a mask without washing hands increases the risk of contamination by 3-5 times). |
| Correct Wearing | 1. Identify the front and back of the mask (waterproof layer facing outward, nose clip metal strip on top). 2. Hold the ear straps with both hands and fully unfold the mask. 3. Press the nose clip firmly to ensure the mask fits snugly. 4. Adjust the ear straps to avoid over-tightening or over-loosening. | 1. Wearing the mask inside out (with the inner layer facing outward). 2. Not tightening the nose clip tightly, causing air leaks. 3. Touching the outer surface of the mask (which may contaminate the mask with pathogens). | A loose nose clip can result in air leakage exceeding 50% and a reduction in filtration efficiency by over 30% (ASTM test data). |
| Management During Use | 1. Wear the mask continuously for ≤ 4 hours (replace immediately if wet or contaminated). | 1. Reuse disposable masks. | Spraying with alcohol can deactivate the electrostatic adsorption of meltblown fabric, reducing filtration efficiency by 90% (NIH study). |
| 2. Avoid frequent touching of the mask. | 2. Pull the mask up to the chin or hang it over the ears. | ||
| 3. If adjustments are necessary, disinfect hands or use disinfectant wipes. | 3. Spray with alcohol for disinfection before continuing use (to destroy the electrostatic layer). | ||
| Removal and Disposal | 1. Remove the mask by touching only the ear or headband. | 1. Remove the mask by grasping the outer layer directly. | The outer layer of the mask may carry live viruses (COVID-19 can survive on non-woven fabrics for 7 days). |
| 2. Dispose of immediately in a designated trash can or sealed bag. | 2. Discard in public areas. | ||
| 3. Wash hands or disinfect again after removal. | 3. Place the used mask in a pocket or bag for reuse. | ||
| Special Scenarios | Medical Procedures: Do not adjust the mask during surgery. For aerosol procedures (such as intubation), choose N95 or medical protective masks for children: - Choose a child-specific size and supervise the child for ≤ 2 hours. | 1. Use non-medical masks in high-risk environments. 2. Wear adult-sized masks on children (poor seal). 3. Prolonged use by patients with respiratory diseases can lead to hypoxia. | Due to the large variations in facial size, adult masks can have leak rates as high as 60%. |
| Effect Verification | Simple Test: - Cover the mask with both hands and exhale to check for leaks around the edges. Professional Test: - Medical institutions can use a fluorescent test to test the seal. | Ignore obvious leaks or increased breathing resistance. | A leak rate >10% indicates a mask's actual filtration efficiency is reduced by more than 50% (OSHA standards). |
3.Storage conditions of disposable medical masks
The protective performance of disposable medical masks depends not only on their production process and quality standards, but also on the storage conditions. Improper storage may cause material aging, decreased filtration efficiency, and even the breeding of microbial contamination. The following are detailed specifications for the storage of disposable medical masks:
(1) Storage environment requirements
1) Temperature and humidity control Temperature: It is recommended to store in a dry environment of 15°C~30°C, avoiding high temperature (>40°C) or low temperature (<0°C) environments. High temperature effects: may cause the electrostatic attenuation of meltblown fabrics and reduced filtration efficiency; non-woven fabrics become brittle and the sealing is reduced. Low temperature effects: may harden the material and easily break when worn. Humidity: Relative humidity should be ≤70%, avoid humid environments (such as bathrooms and kitchens). Excessive humidity: may breed mold or bacteria, increasing the risk of use.
2) Light and ventilation Storage away from light: Avoid direct sunlight or ultraviolet radiation (such as near windows, in cars) to prevent oxidation and degradation of the material. Good ventilation: The storage area must maintain air circulation to prevent moisture accumulation in the enclosed space.
(2) Packaging and storage methods
1) Storage in original packaging Unopened masks should be kept in the original factory sealed packaging to prevent dust and microbial contamination. It is recommended to use damaged or opened masks as soon as possible or store them in sealed bags/boxes.
2) Classified storage Home storage: They can be placed in drawers, storage boxes or special mask storage bags, away from chemicals (such as disinfectants and perfumes). Medical/institutional storage: They can be stored by batch and expiration date, following the "first in, first out" principle. Store in a clean area or a special cabinet for medical supplies to avoid contact with contaminated items.
(3) Shelf life and expiration date Unopened masks:
The shelf life is usually 2 to 3 years (based on the product label). After expiration, the filtration efficiency and material strength may decrease. Opened masks: It is recommended to use them within 1 month. If exposed to a humid or polluted environment, they need to be replaced as soon as possible.
(4) Special precautions
No contact with contamination sources: Avoid direct contact with dirty hands and contaminants (such as coins, keys).
Avoid squeezing and deformation: Do not overload when stacking to prevent the metal strip of the nose clip from deforming or the ear strap from breaking.
Safety for children and pets: Store in a place out of reach of children and pets to prevent misuse or accidental ingestion.
(5) Handling of abnormal situations
Stop using if the following conditions are found:
The packaging is damp, damaged or moldy.
The mask has an odor, discoloration or obvious stains.
The material becomes hard, delaminated or loses elasticity.
Disposable medical mask storage environment requirements table:
| Storage Conditions | Specific Requirements | Possible Impacts | Recommended Actions |
| Temperature | 15°C~30°C (Avoid extreme high or low temperatures) | High temperatures (>40°C): Electrostatic discharge of the meltblown fabric degrades, reducing filtration efficiency. Low temperatures (<0°C): The material becomes brittle and prone to cracking. | Avoid storage in vehicles, near heaters, or in freezers. |
| Humidity | Relative humidity ≤70% (dry environment) | Excessive humidity: Bacteria and mold grow, reducing protective effectiveness. | Store in sealed bags or moisture-proof containers, away from bathrooms and kitchens. |
| Light | Store away from light (direct sunlight and UV rays). | UV rays: Accelerate material aging, causing the non-woven fabric to turn yellow and become brittle. | Store in a cool drawer, locker, or in the original packaging. |
| Ventilation | Maintain good air circulation; avoid confined, humid spaces. | Enclosed environments: Moisture accumulates, increasing the risk of contamination. | Regularly inspect the storage area to ensure there is no musty odor or water damage. |
| Packaging Condition | Unopened: Keep in original sealed packaging. Opened: Store in sealed bags/boxes. | Damaged packaging: Increased risk of contamination from dust and microorganisms. | Mark the date after opening and use within one month. |
| Storage Methods | Store flat or upright to avoid deformation due to heavy pressure. | Excessive compression: The metal strip of the nose clip may deform and the ear loop may break. | In medical institutions, use shelving for tiered storage. Avoid excessive stacking at home. |
| Chemical Contamination Protection | Keep away from chemicals such as disinfectants, perfumes, and pesticides. | Chemical Contact: Corrosion or release of harmful substances. | Store separately, away from cleaning supplies. |
| Shelf Life Management | Unopened: 2-3 years (based on product labeling). Opened: Recommended use within one month. | Expired: Reduced filtration efficiency and ineffective protection. | Check inventory regularly and use on a "first-in, first-out" basis. |
| Special Location Requirements | Medical Institutions: Store in a clean area or dedicated cabinet. Homes: Keep away from children and pets. | Children's Contact: Risk of misuse or ingestion. | Use a locked storage box or store in a high place |
4.Guidelines for handling abnormal situations of disposable medical masks
(1) Common abnormalities and treatment measures
Abnormal packaging
Damaged packaging: Immediately stop using the masks in this batch and check whether the adjacent packaging is damaged
Wet packaging: Discard the entire package and check the humidity of the storage environment
Molded packaging: Discard the entire batch of masks and thoroughly clean the storage area
Abnormal appearance of masks
Obvious stains: Discard directly and trace the source of contamination
Color change: Stop using and check the lighting conditions of the storage environment
Structural deformation: Discard the deformed nose clip and loose ear straps
Abnormal material
Hardened material: May be caused by low temperature or aging and should be discarded
Delamination and detachment: Stop using immediately and check the production batch
Odor: Discard and check the storage environment for pollutants
(2) Treatment of abnormal performance
Decrease in filtration efficiency: Replace immediately when breathing resistance is significantly reduced, and regularly sample and inspect when using in batches
Abnormal wearing: Replace with a suitable model when it cannot fit the face tightly , if skin irritation occurs, the material type should be changed
(3) Abnormal handling of storage environment
Temperature and humidity exceed the standard: immediately move to a qualified environment, and the affected masks need to be sampled and tested before deciding whether to use
Chemical contamination: Contaminated by disinfectants, etc. should be discarded in batches, and isolation measures for storage areas should be strengthened
(4) Handling process
Isolation: Abnormal masks should be immediately removed from the use area
Evaluation: Professionals will determine the scope of impact
Record: Detailed record of abnormal conditions and handling processes
Improvement: Analyze the causes and improve the management system
(5) Precautions
Personal protection should be taken when handling abnormal masks
Abnormal medical masks must be handled as medical waste
Establish an abnormal situation handling file for reference
Regularly inspect and maintain the storage environment
(6) Preventive measures
Strictly implement the first-in-first-out principle
Establish a regular inspection system
Special training for key personnel
Set up dedicated storage monitoring equipment
Guidelines for handling abnormal situations:
| Abnormalities | Possible Causes | Handling Methods |
| Damp/Mold Packaging | Excessive Humidity in Storage | Discard immediately and replace with a new mask from a new batch |
| Mask has an odor or discoloration | Material degradation or chemical contamination | Stop use and inspect storage conditions |
| Deformed nose clip/broken ear strap | Deformation due to compression or high temperature | Scrap and adjust storage methods |
5. Disposal of disposable medical masks after use
Disposable medical masks need to be properly disposed of after use to avoid cross infection or environmental pollution. The following are the correct disposal methods:
(1). General population (no fever, cough, etc.)
When taking off the mask: avoid touching the outside of the mask, only touch the ear loop or tie part. Folding mask: fold the mask in half (contaminated side facing inward), wrap the folded mask with the ear loop or tie to avoid direct contact with the contaminated surface. Disposal: put it in a sealed bag or directly put it into a dedicated medical waste trash can (such as the hospital yellow trash can). If there is no dedicated trash can, it can be thrown into an ordinary trash can and then wash hands in time. Wash hands: Wash hands immediately with soap or hand sanitizer after handling the mask, or disinfect with hand sanitizer.
(2). Suspected or confirmed infected persons
Sealed treatment: put the mask in a sealed bag (such as a plastic bag), spray a small amount of disinfectant (such as chlorine-containing disinfectant) and then discard it into the medical waste trash can. Professional treatment: If in a medical institution, it must be handed over to professionals for disposal according to the medical waste process.
(3). Notes
The following behaviors are prohibited: random discarding (such as on the ground, in public areas). Reusing disposable masks. Burning or shredding masks (may cause secondary pollution or safety hazards).
Environmental protection tips: Masks are medical waste and cannot be recycled through ordinary treatment. They should be discarded separately from other household waste.
(4). Disposal by medical institutions
Strictly follow the "Medical Waste Management Regulations" and classify masks as infectious waste (yellow garbage bags) and have them destroyed by professional institutions.
Proper disposal of masks is an important part of preventing the spread of viruses. Please be sure to follow the standard procedures!
6.How long can disposable medical masks be used?
Disposable medical masks are commonly used protective equipment in daily life, especially during the flu season, air pollution or epidemic period. Correct use and replacement of masks are essential for health. However, many people have doubts about the use time of masks: How long can they be used? Can they be reused? How to judge whether they need to be replaced?
(1) Standard use time of disposable medical masks
1). General use recommendations
According to the recommendations of the World Health Organization (WHO) and national CDCs:
Continuous wear for no more than 4 hours: In ordinary environments (such as offices, shopping malls, public transportation), it is recommended to replace them every 4 hours.
Single use for no more than 8 hours: If it is only worn for a short time (such as going out to buy groceries, picking up express delivery), and the mask is not contaminated, the use time can be appropriately extended, but the cumulative time should not exceed 8 hours.
Why 4 hours?
Wearing for a long time will cause the electrostatic adsorption capacity of the filter layer (meltblown cloth) of the mask to decrease, reducing the protective effect.
The exhaled water vapor will make the mask moist, increasing the risk of bacterial growth.
2). Frequency of replacement in special circumstances
High-risk environments (hospitals, crowded places): It is recommended to replace every 2-4 hours.
The mask is damp, contaminated or damaged: If it is contaminated by sweat, rain, droplets, or is damaged or the nose clip is loose, it should be replaced immediately.
After contact with suspected/confirmed infected persons: Even if it is worn for a short time, a new mask should be replaced.
(2) In what situations must the mask be replaced?
Even if it has not been worn for 4 hours, it should be replaced immediately in the following situations:
The mask becomes wet (such as due to breathing, sweat, rain).
The breathing resistance increases significantly (indicating that the filter layer has been blocked by particulate matter).
The mask is damaged, deformed or cannot fit the face (such as the nose clip is broken or the ear straps are loose).
After touching the inside of the mask (hands may contaminate the inside of the mask).
After using it in a medical environment or high-risk place (such as a hospital, nucleic acid testing point).
(3) Incorrect use:
These practices will reduce the protective effect. Reuse after disinfection with alcohol: Alcohol will destroy the electrostatic adsorption ability of meltblown cloth, which will greatly reduce the filtration efficiency. Hanging around the neck or putting it in the pocket after taking it off: The outside of the mask may be contaminated with viruses, and it is easy to contaminate clothes or skin if it is left lying around. Continue to use after washing or exposure to the sun: The material of disposable masks is not resistant to washing, and exposure to the sun cannot restore the filtration effect. Wearing multiple layers: Wearing multiple masks may affect the airtightness and increase the risk of leakage.
(4) How to extend the service life of the mask? (Emergency plan for special circumstances)
When masks are in short supply (such as during the epidemic), the following methods can be used to appropriately extend the use time (but still need to be cautious): Use according to occasions Use new masks in high-risk places (hospitals, public transportation), and the use time can be appropriately extended in low-risk environments (outdoor walking). Proper storage of temporarily removed masks When taking them off for a short time, they can be hung in a ventilated place or placed in a clean paper bag to avoid folding and contamination. Avoid frequent wearing and taking off. Reduce unnecessary adjustments to avoid hand contamination of the inside of the mask.
Note: These methods are only suitable for emergency situations and should not be relied upon long-term. The protective effect will still decrease over time.
7.Frequently asked questions about disposable medical masks
Disposable medical masks are an essential tool for daily protection, but many people still have questions about their use. Below are frequently asked questions about disposable medical masks and their professional answers to help you use them correctly and ensure effective protection.
(1). What is the difference between disposable medical masks and surgical masks?
Disposable medical masks (ordinary medical masks):
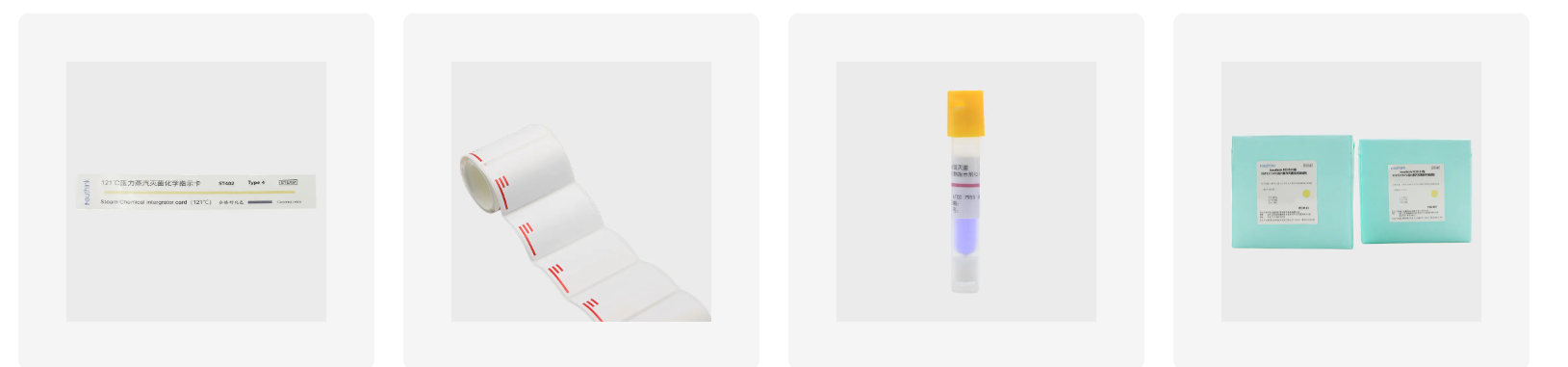
Compliant standard: YY/T 0969-2013 (China) or ASTM F2100-19 Level 1 (International).
Main function: Blocks droplets and dust, suitable for daily protection (such as in public places and general travel).
Filtration efficiency: Bacterial filtration efficiency (BFE) ≥ 95%, but does not provide liquid penetration resistance.
Surgical masks:
Compliant standard: YY 0469-2011 (China) or ASTM F2100-19 Level 2/3 (International).
Main function: In addition to blocking droplets, they also provide protection against blood and body fluid splashes, suitable for use in medical environments (such as hospitals and clinics). Filtration efficiency: BFE ≥ 95%, PFE (Particle Filtration Efficiency) ≥ 30%, and a liquid-resistant layer.
Summary: Surgical masks offer greater protection, but ordinary medical masks are sufficient for daily use.
(2). How long can disposable medical masks be used? Can they be reused?
Recommended use duration:
Normal environments: 4 hours (e.g., work, shopping).
High-risk environments (hospitals, crowded places): 2-4 hours.
Replace immediately if damp, contaminated, or damaged.
Can they be reused?
Not recommended, but in emergencies, the following measures can be taken:
When removing the mask briefly, hang it in a well-ventilated area or place it in a clean paper bag.
Avoid touching the inside of the mask. Keep the total usage to no more than 8 hours.
(3). Does wearing the mask upside down affect its protection?
Yes!
The white side (water-absorbing layer) should face inward, close to your mouth and nose, to absorb exhaled moisture.
The blue/green side (water-repellent layer) should face outward to block droplets and dust. Wearing the mask upside down may cause dampness and discomfort, and reduce protective effectiveness.
(4). Can masks be disinfected with alcohol or UV light?
Not recommended!
Alcohol: It will destroy the electrostatic adsorption capacity of the meltblown fabric, reducing filtration efficiency.
UV light: It may age the material and fail to completely kill viruses inside.
Correct: Disinfection of disposable masks is not recommended; they should be replaced immediately.
(5). Can children wear adult masks?
Not recommended:
Adult masks do not fit children's faces properly and provide less protection.
Select a child-specific mask (compliant with GB/T 38880-2020).
(6). What should I do if I experience skin allergies or acne after wearing a mask?
Cause: Prolonged wearing creates a humid and hot environment, breeding bacteria, or friction irritation.
Solution:
Remove the mask and allow it to air out every two hours.
Opt for a breathable mask (such as a three-layer non-woven + meltblown fabric).
Apply moisturizer before wearing and avoid heavy makeup.
(7). What is the purpose of the nose clip on a mask? How do you properly shape it?
Purpose: Ensures a tight fit between the mask and the face to prevent air leaks.
Proper shaping method:
After putting on the mask, use both hands to press the nose clip to fit the contour of the nose bridge.
Check for gaps (if leaks occur, adjust or replace).
(8). How should a used mask be disposed of?
General public:
Fold (contaminated side facing inward), discard in the trash, and wash hands.
Suspected/confirmed infected individuals:
Seal the mask and dispose of it as medical waste (e.g., in a yellow trash can).
Do not: Discard, incinerate, or shred (may cause secondary contamination).
(9). Why do glasses fog up when wearing a mask? How can this be fixed?
Cause: The top of the mask is not properly fitted, causing exhaled air to impact the lenses upward.
Solution:
Adjust the nose clip to ensure a tight fit on the nose bridge.
Press the glasses against the mask.
Use anti-fog spray or anti-fog cloth for glasses.
(10). Do disposable medical masks protect against PM2.5 and viruses?
PM2.5 protection: Ordinary medical masks have limited filtering capabilities for non-oily particles. KN95/N95 masks are recommended.
Viral protection: They can block droplet transmission (the primary viral vector), but cannot filter 100% of aerosols.
Summary
Notes on proper use of disposable medical masks:
Distinguish the front and back to ensure a tight fit.
Change every four hours and discard immediately if damp or contaminated.
Do not reuse or disinfect to prevent loss of protection.
Use masks specifically designed for children to avoid loose fit.



 English
English Español
Español Français
Français










 CONTACT US
CONTACT US