laparoscopic stapler Manufacturers
Eray MedTech Laparoscopic Stapler
Intended Use
For the dissection, resection, and anastomosis of pulmonary, bronchial, gastric, and intestinal tissues in open and endoscopic surgery.
Operational Principle
Integrates simultaneous cutting & stapling via a tissue-cutting blade assembly and a stapling cartridge that deploys surgical-grade titanium staples.
Clinical Outcomes
Achieves hemostasis during transection.

With a building area of 20,310 square metres, the company has a class 100,000 purified production workshop, a class 10,000 microbiology testing room, a local class 100 physical and chemical laboratory, and a standardised storage system for raw materials and finished products.
Since the initial batch of products were launched in 2013, Eray has continuously enriched its product categories. Our products have covered protective masks, nursing consumables, sensory control consumables, surgical instruments, providing safe, efficient and environmentally friendly disposable medical solutions for medical institutions worldwide.
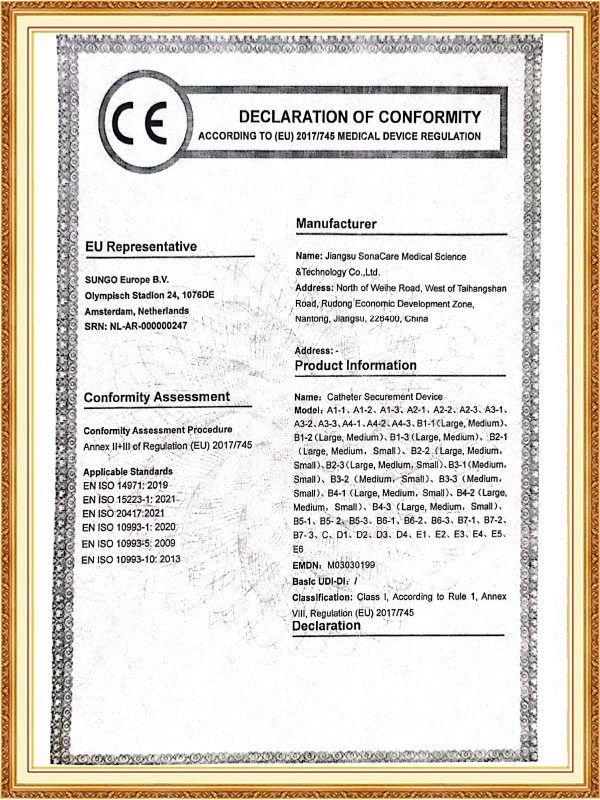
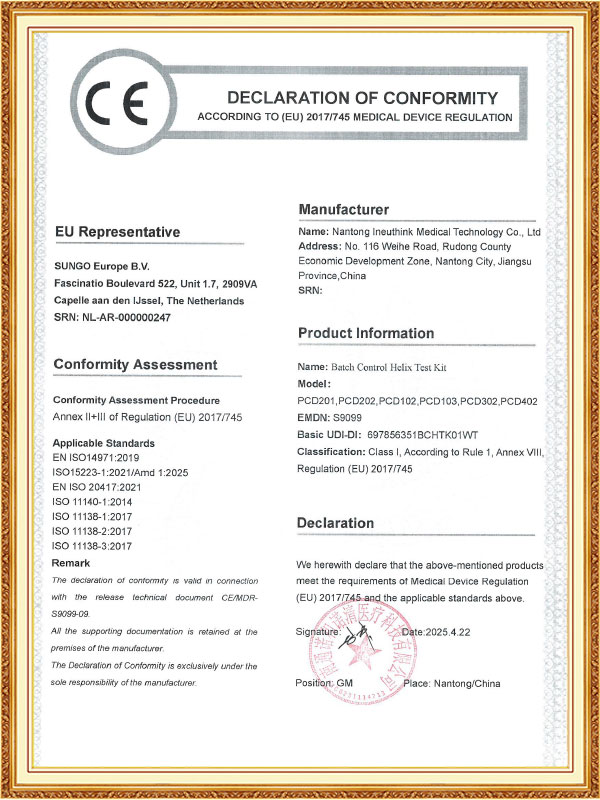
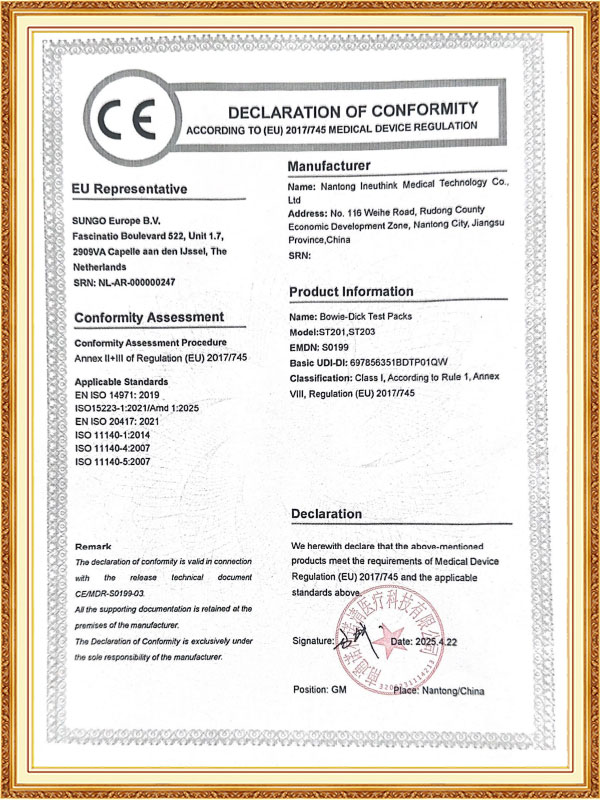
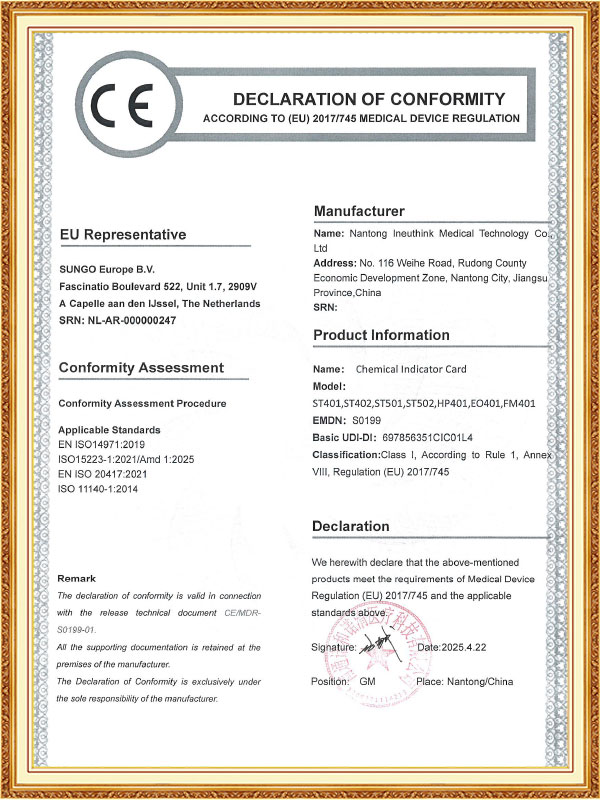
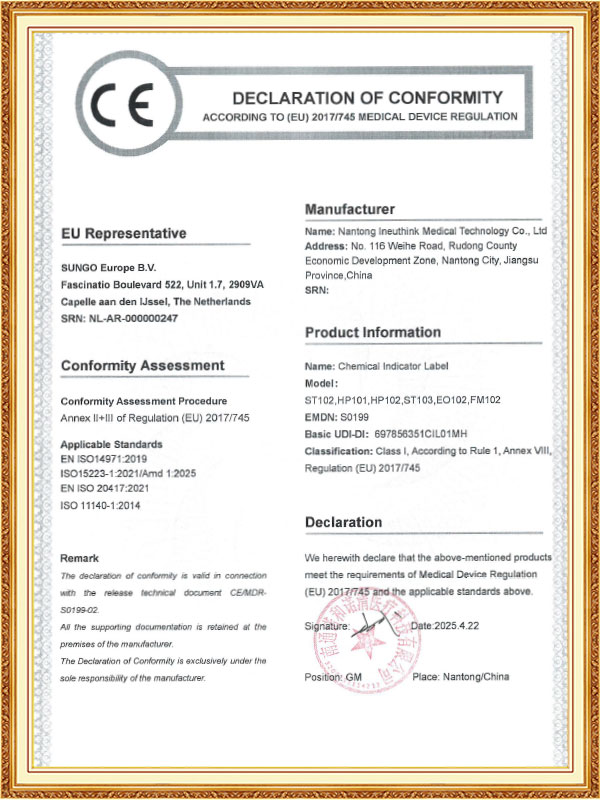
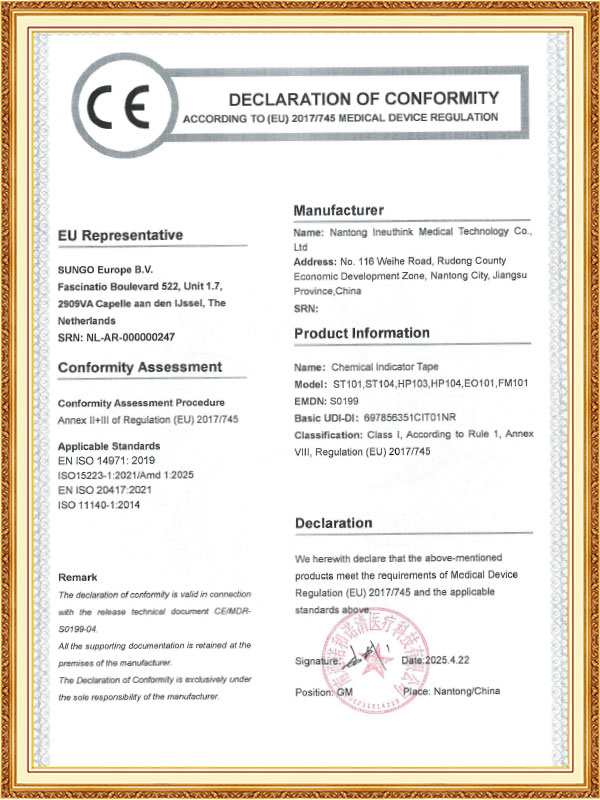
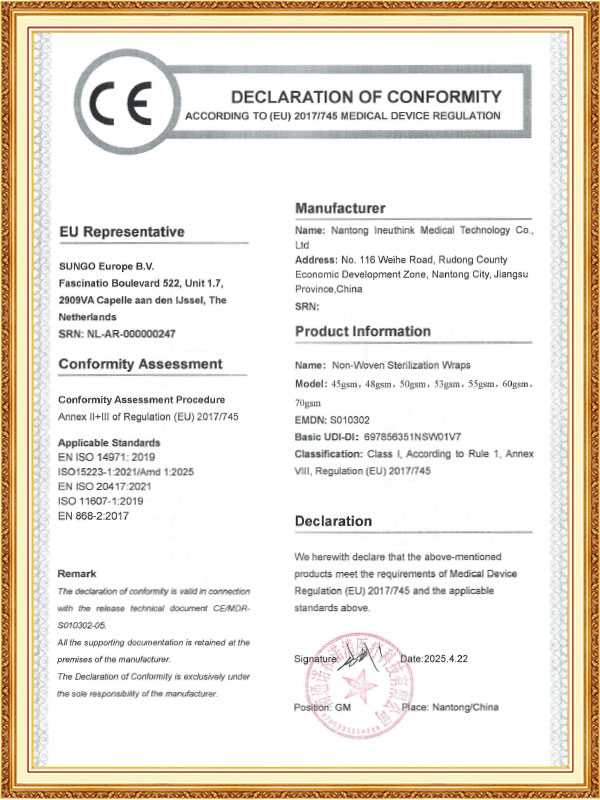
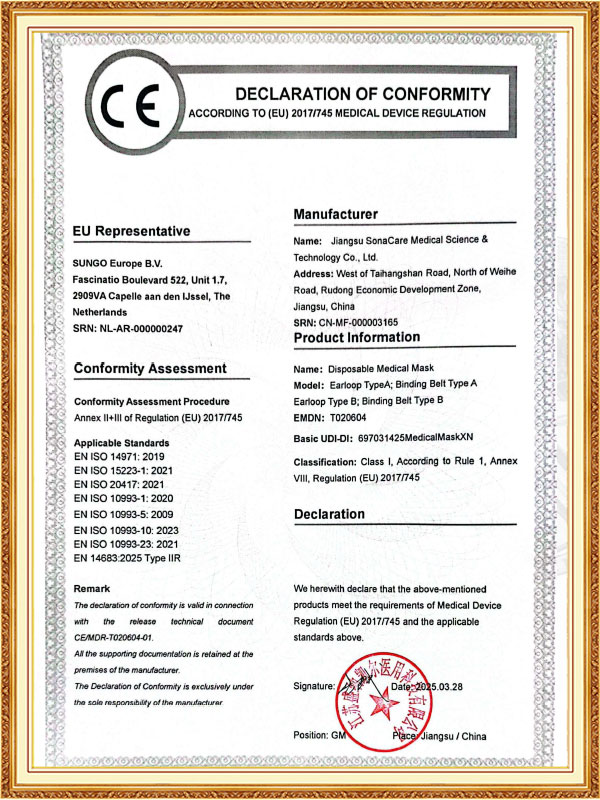
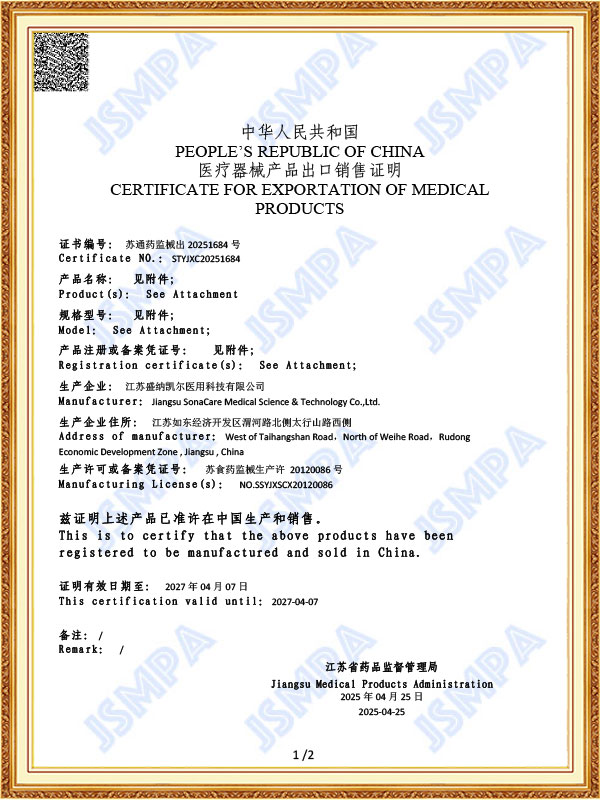
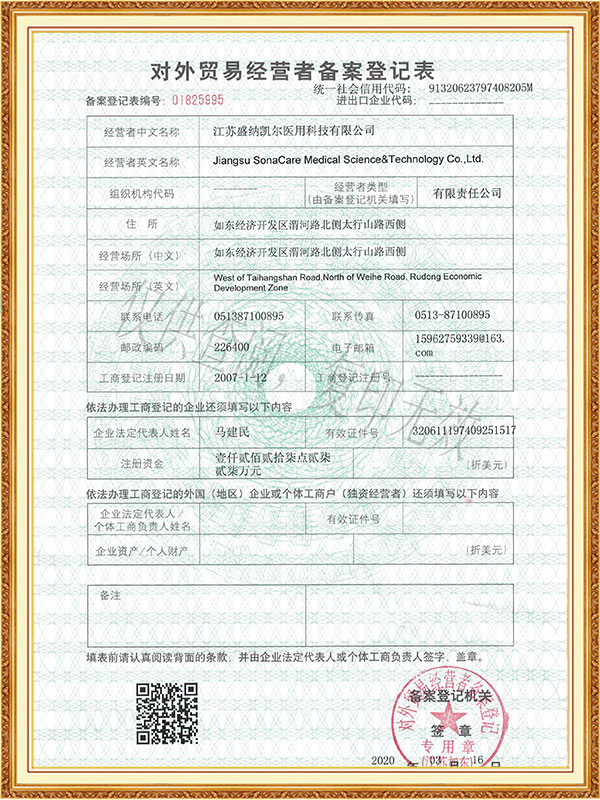
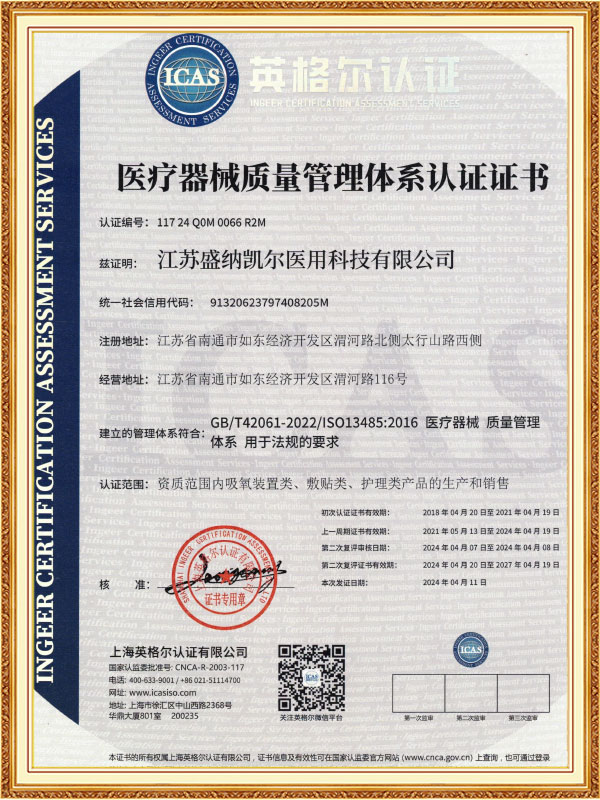
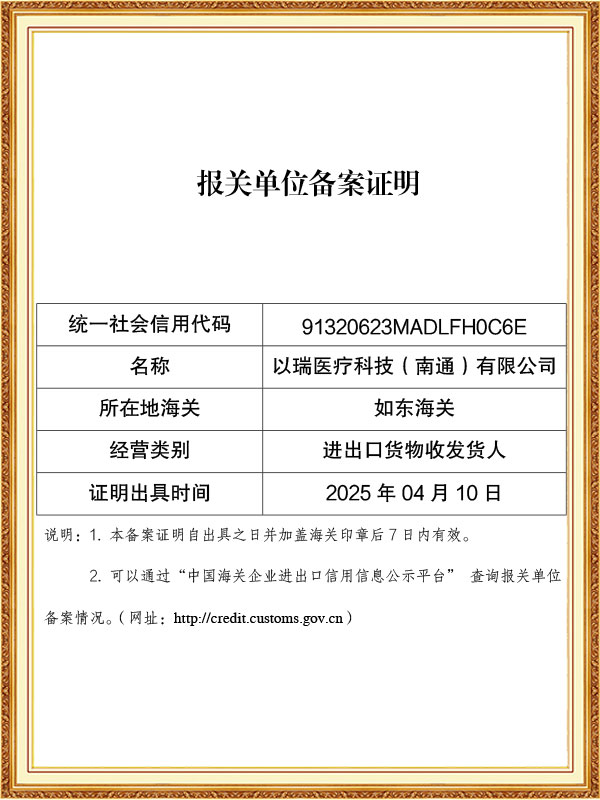
As a professional OEM laparoscopic stapler Manufacturers and ODM laparoscopic stapler Factory, The company has passed ISO 13485 and other quality system certifications, and some of its products have obtained CE certification and FDA filing permits, and has established long-term cooperative relationships with many domestic and foreign medical institutions and distributors.
-
Feb 27. 2026
Can Optical Trocars Reduce the Risk of Organ Injury?Optical Trocars Significantly Reduce Organ Injury Risk Yes, optical trocars can significantly reduce the risk of organ injury during laparoscopic surgery by allowing surgeons to visualize tissue layers in real time as the instrument passes through the abdominal wall. Unlike blin...
Read More -
Feb 20. 2026
What is an Optical Trocar and Why is it Essential in Medical Procedures?What is an Optical Trocar and Why is it Essential in Medical Procedures? An optical trocar is a specialized surgical instrument used primarily in minimally invasive procedures. It combines the functions of a trocar and a visual scope, allowing surgeons to create an access point ...
Read More -
Feb 13. 2026
What Are the Common Problems With Medical Trocars and How to Avoid Them?What Are the Most Common Problems With Medical Trocars? The most common problems with medical trocars include insertion injuries, gas leakage, dull blades, instability, and contamination risks. These issues can compromise surgical safety, increase operating time, and raise posto...
Read More
Laparoscopic staplers utilize a slender instrument shaft and a sophisticated end effector mechanism to precisely transmit the surgeon's hand movements to the surgical site, enabling precise three-dimensional suturing under the guidance of a two-dimensional monitor.
Technically, modern laparoscopic staplers are the culmination of mechanical engineering and surgical expertise. The instrument typically consists of a control handle, a flexible shaft, and a suturing head. The ergonomic design of the control handle allows for natural and comfortable control by the surgeon, while the flexible steerability of the shaft ensures access to any corner of the abdominal cavity. The precise suturing head handles the entire process, including needle threading, threading, and knotting. Some models feature a 360-degree rotatable design, compatible with needles of varying angles, allowing surgeons to perform suturing at various angles in an ergonomically optimized position.
Laparoscopic staplers are constructed from medical-grade stainless steel and special alloys to ensure sufficient strength and durability. A micro-gear transmission system and sophisticated mechanical structure ensure accurate and stable motion transmission. The innovative self-locking needle design and automatic thread trimmer significantly enhance surgical efficiency. Some products also incorporate tactile feedback systems, allowing surgeons to sense tissue tension and suture tightness, nearly recreating the feel of open surgery. In gastrointestinal surgery, it enables precise intestinal anastomosis; in gynecological surgery, it allows for delicate uterine or fallopian tube suturing; and in urology, it enables precise reconstruction after prostatectomy. Compared to traditional open surgery, suturing performed using a laparoscopic stapler is less invasive, more precise, and more effective.
Laparoscopic stapler maintenance is crucial for ensuring the smooth performance of minimally invasive surgery, and strict maintenance protocols are essential. After daily use, the detachable components should be disassembled immediately. A neutral enzymatic cleaner and a soft-bristled brush should be used to thoroughly clean the stapler head, firing mechanism, and joints, paying particular attention to removing any residual tissue from the stapler slot and stapler pusher. After cleaning, the internal components should be dried with a high-pressure air gun to prevent residual moisture from rusting. Weekly inspections should be conducted to ensure the smoothness of the firing mechanism and the firing force is within the specified range, ensuring that each firing fully ejects the staples. Lubrication and maintenance of precision components are crucial, and medical-grade grease should be used to regularly maintain the joints and mechanical transmission mechanisms to maintain smooth and flexible operation.
The instrument must be completely disassembled before sterilization. The appropriate sterilization method should be selected based on the material properties. High-temperature resistant components should be sterilized with high-pressure steam at 134°C, while precision electronic components should be sterilized with ethylene oxide or hydrogen peroxide low-temperature plasma. Staplers should be stored in a dedicated instrument case to prevent deformation and compression, and in a dry environment. Before each surgery, a functional test is performed to check whether the staple cartridge is properly loaded and the firing resistance is normal, ensuring that the equipment is in optimal working condition. A comprehensive usage record is established, detailing each maintenance and sterilization cycle. Staplers that have reached their service life are promptly scrapped and replaced. Through scientific and standardized maintenance management, not only can the service life of the equipment be extended, but the safety and reliability of each surgery can also be ensured, providing patients with high-quality minimally invasive surgical treatment.



 English
English Español
Español Français
Français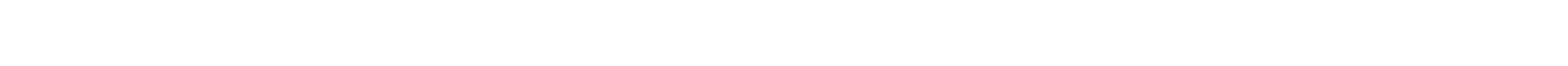












 CONTACT US
CONTACT US