Medical Devices & Consumables Suppliers

With a building area of 20,310 square metres, the company has a class 100,000 purified production workshop, a class 10,000 microbiology testing room, a local class 100 physical and chemical laboratory, and a standardised storage system for raw materials and finished products.
Since the initial batch of products were launched in 2013, Eray has continuously enriched its product categories. Our products have covered protective masks, nursing consumables, sensory control consumables, surgical instruments, providing safe, efficient and environmentally friendly disposable medical solutions for medical institutions worldwide.
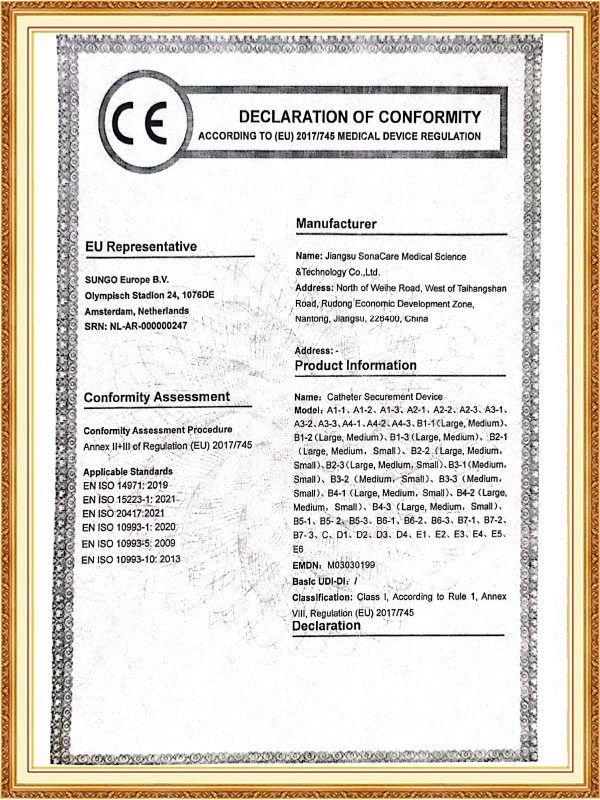
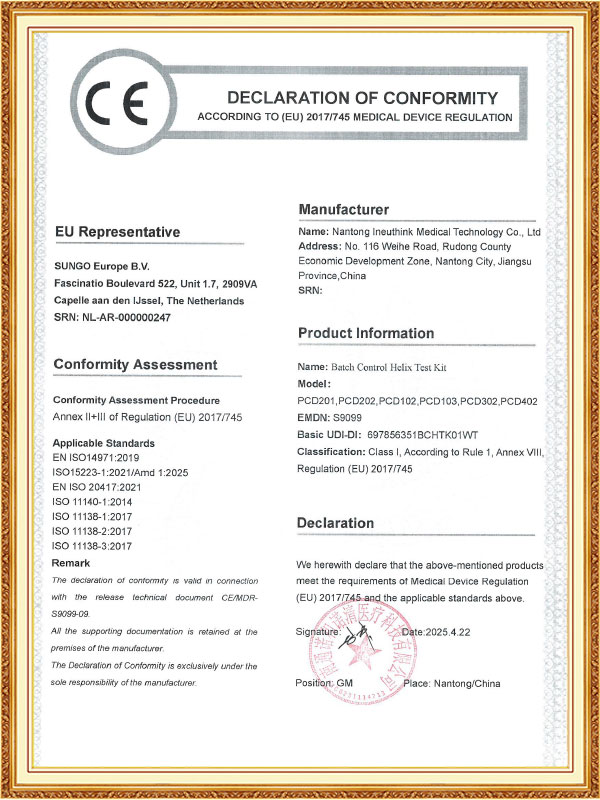
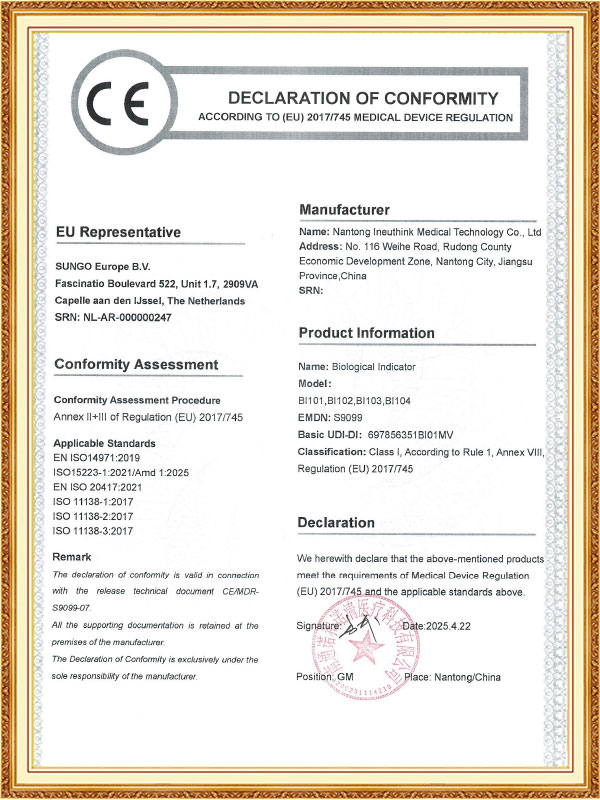
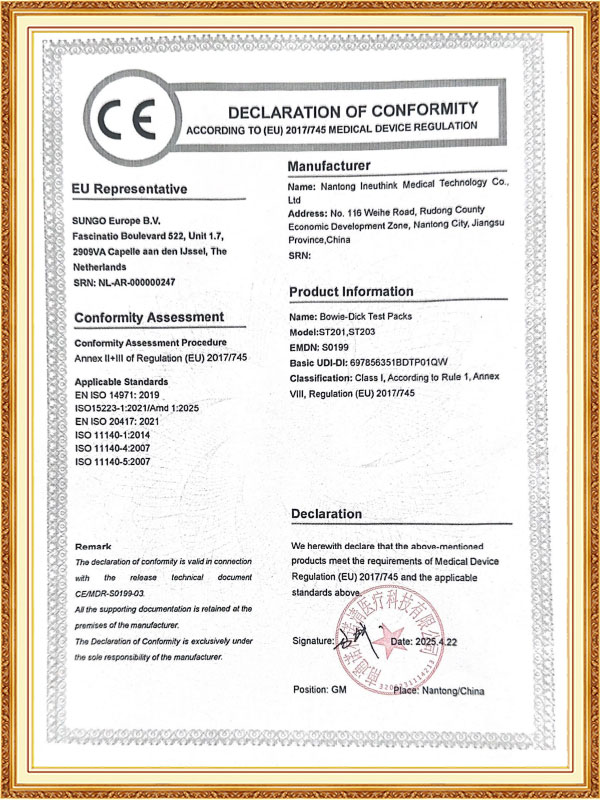
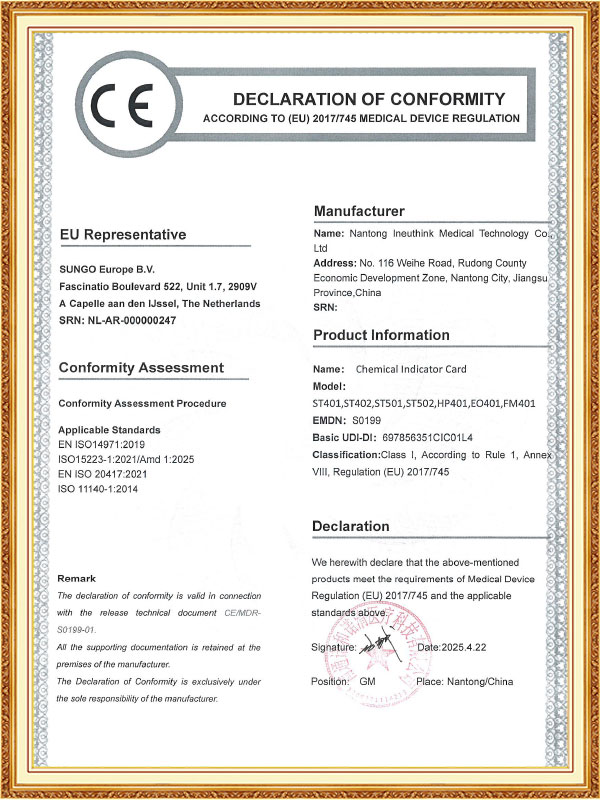
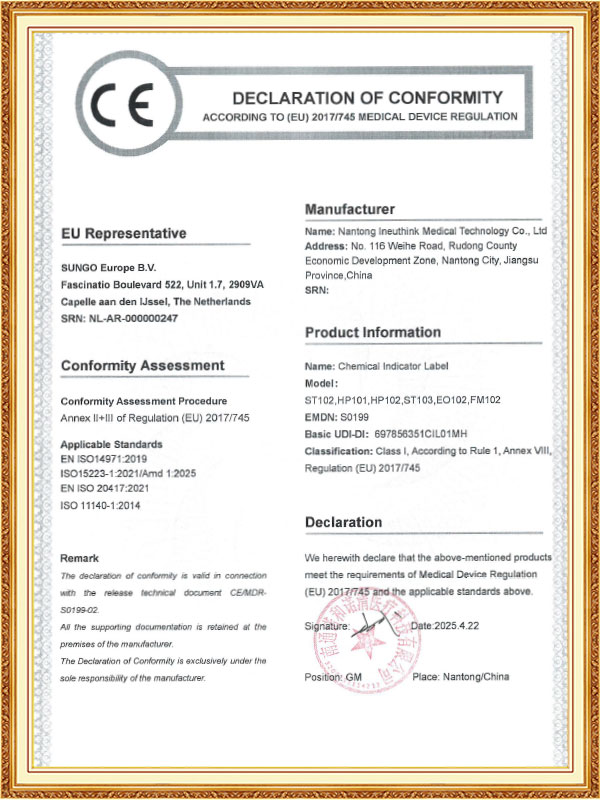
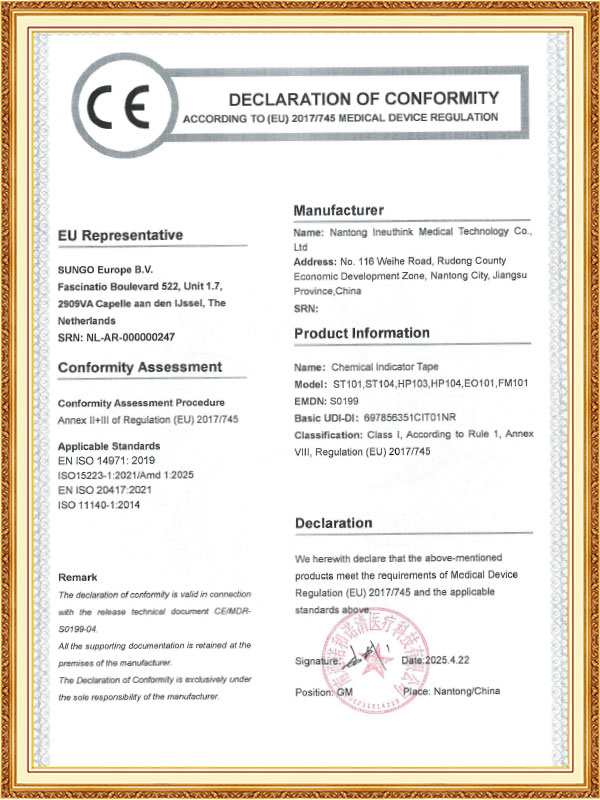
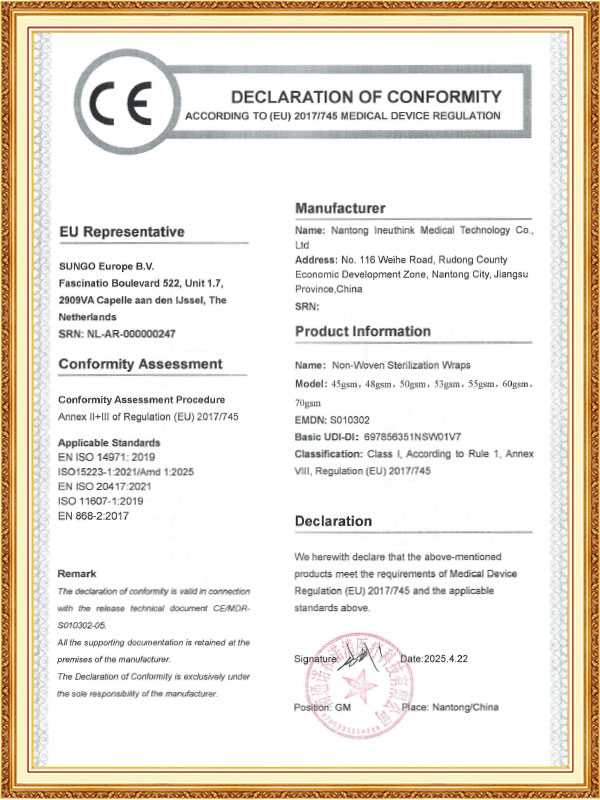
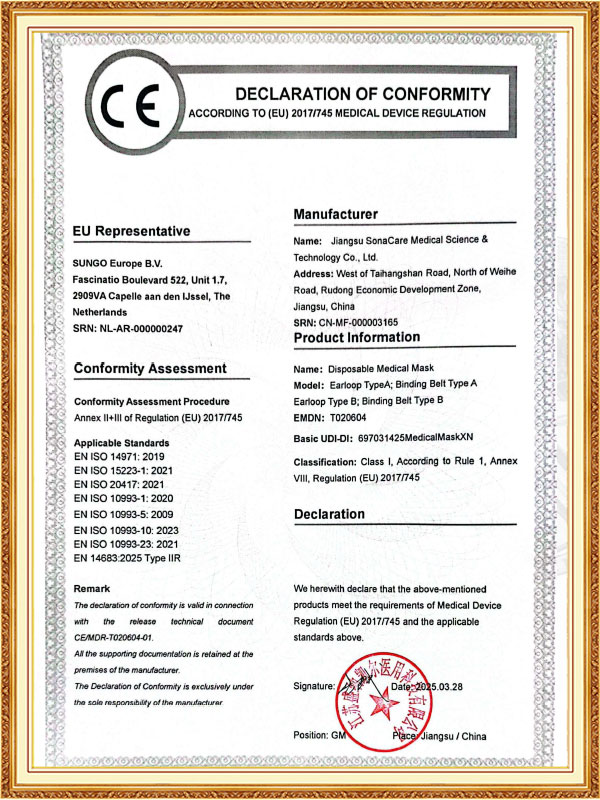
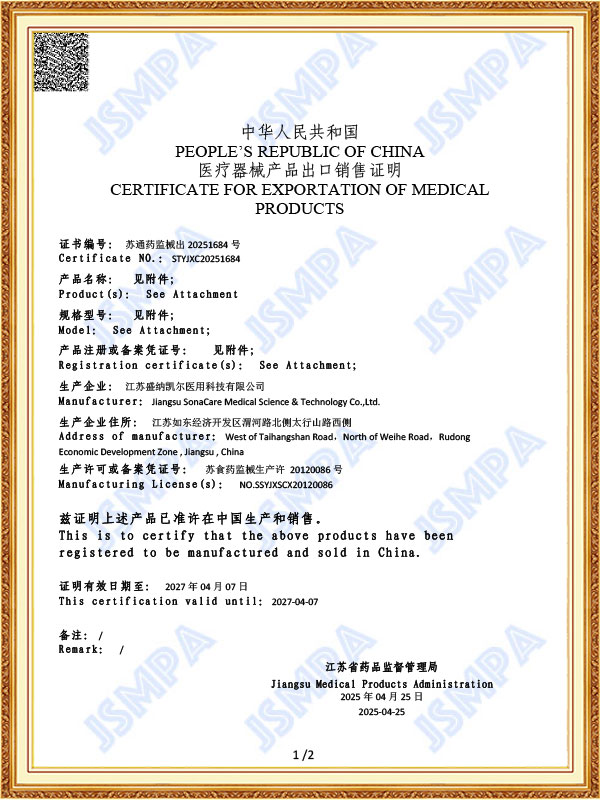
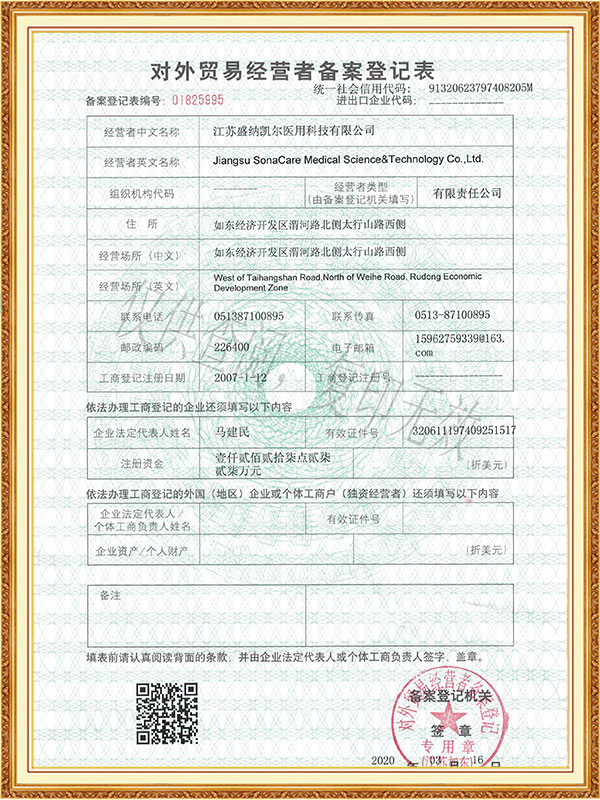
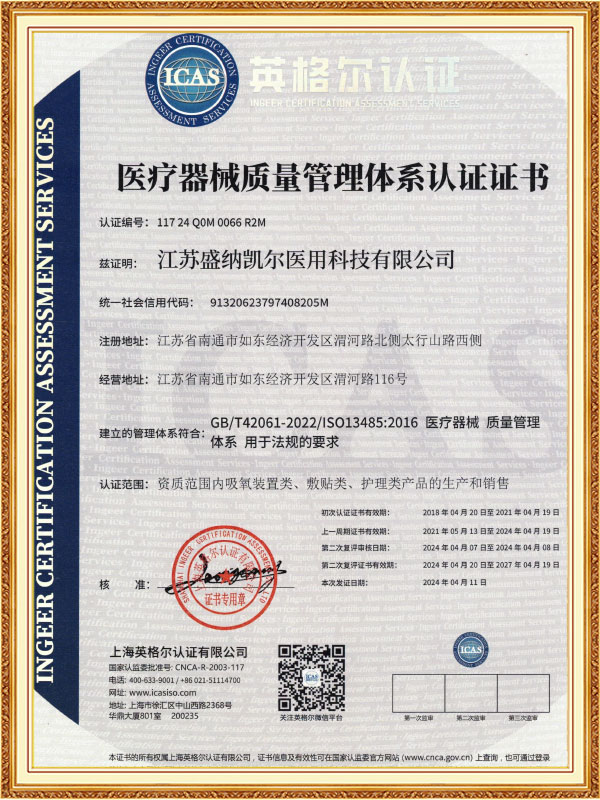
As a professional OEM Medical Devices & Consumables Suppliers and ODM Medical Devices & Consumables Company, The company has passed ISO 13485 and other quality system certifications, and some of its products have obtained CE certification and FDA filing permits, and has established long-term cooperative relationships with many domestic and foreign medical institutions and distributors.
-
Feb 27. 2026
Can Optical Trocars Reduce the Risk of Organ Injury?Optical Trocars Significantly Reduce Organ Injury Risk Yes, optical trocars can significantly reduce the risk of organ injury during laparoscopic surgery by allowing surgeons to visualize tissue layers in real time as the instrument passes through the abdominal wall. Unlike blin...
Read More -
Feb 20. 2026
What is an Optical Trocar and Why is it Essential in Medical Procedures?What is an Optical Trocar and Why is it Essential in Medical Procedures? An optical trocar is a specialized surgical instrument used primarily in minimally invasive procedures. It combines the functions of a trocar and a visual scope, allowing surgeons to create an access point ...
Read More -
Feb 13. 2026
What Are the Common Problems With Medical Trocars and How to Avoid Them?What Are the Most Common Problems With Medical Trocars? The most common problems with medical trocars include insertion injuries, gas leakage, dull blades, instability, and contamination risks. These issues can compromise surgical safety, increase operating time, and raise posto...
Read More
In modern healthcare, protection, disinfection, and sterilization are core components of ensuring patient safety and quality of care. Medical protection, disinfection, and sterilization involve numerous equipment and processes, and each step is crucial. From daily protective masks to high-standard sterilization of surgical instruments to aseptic laboratory procedures, scientific equipment and management systems are the cornerstones of medical safety.
Protective masks are the first line of defense for medical staff and patients, primarily used to block the spread of droplets, bacteria, and viruses. Surgical masks and N95/KN95 masks are the most common types. The former is suitable for general protection, while the latter effectively filters tiny airborne particles. Masks are typically made of multi-layered non-woven and meltblown fabrics to ensure both effective protection and breathability. Proper wearing and timely replacement of masks are crucial to maintaining their protective performance.
The usage duration of disposable medical masks needs to be flexibly controlled based on specific circumstances. Generally speaking, under normal use conditions, it is recommended that the mask be worn continuously for no more than four hours, based on a combination of its filtration efficiency and comfort. In high-risk environments such as hospitals, where the risk of exposure to pathogens is higher, it is best to replace the mask every two to four hours. In low-risk settings with good ventilation and few people outdoors, if the mask is kept dry and clean, it can be used for up to six to eight hours, but this is a maximum and should not be exceeded.
In actual use, several key indicators indicate the need for prompt mask replacement: when the mask becomes damp from breathing or perspiration, when it is contaminated by droplets or other contaminants, when it becomes damaged or deformed, compromising its seal, or after leaving high-risk settings such as hospitals. Environmental factors can also affect the duration of use. For example, masks lose their effectiveness more quickly in environments with severe air pollution and high dust levels, while high humidity accelerates the rate at which masks absorb moisture. It's important to note that some people try to reuse disposable masks after disinfecting them to save money, such as by spraying them with alcohol or exposing them to ultraviolet light. These practices are inadvisable because they damage the mask's filter structure and significantly reduce its protective effectiveness. The correct approach is to carry a spare mask with you and replace it promptly when needed. Mask storage is also very important. Unused masks should be kept in a dry, clean environment to avoid moisture and contamination.
Nursing consumables, including disposable items such as gauze, cotton balls, bandages, and medical gloves, are widely used for wound treatment, injections, and daily care. These consumables must meet sterility standards to prevent cross-infection. Furthermore, with growing environmental awareness, the use of biodegradable materials is becoming a growing trend. Aseptic processing solutions are at the core of hospital infection control, encompassing multiple steps including cleaning, disinfection, sterilization, and monitoring. CSSD (Central Sterilization Supply Center) furniture and small equipment, such as instrument recovery carts and wash stations, provide a standardized working environment for aseptic processing. Instrument washer-disinfectors and steam sterilizers are core CSSD equipment. The former uses high-temperature water and chemical cleaning agents to remove organic matter from instruments, while the latter utilizes high-pressure saturated steam to thoroughly kill microorganisms, ensuring the sterility of instruments. Vacuum boiling washing machines are suitable for washing high-temperature-resistant linens, using vacuum boiling technology to improve cleaning efficiency and sterilization effectiveness.
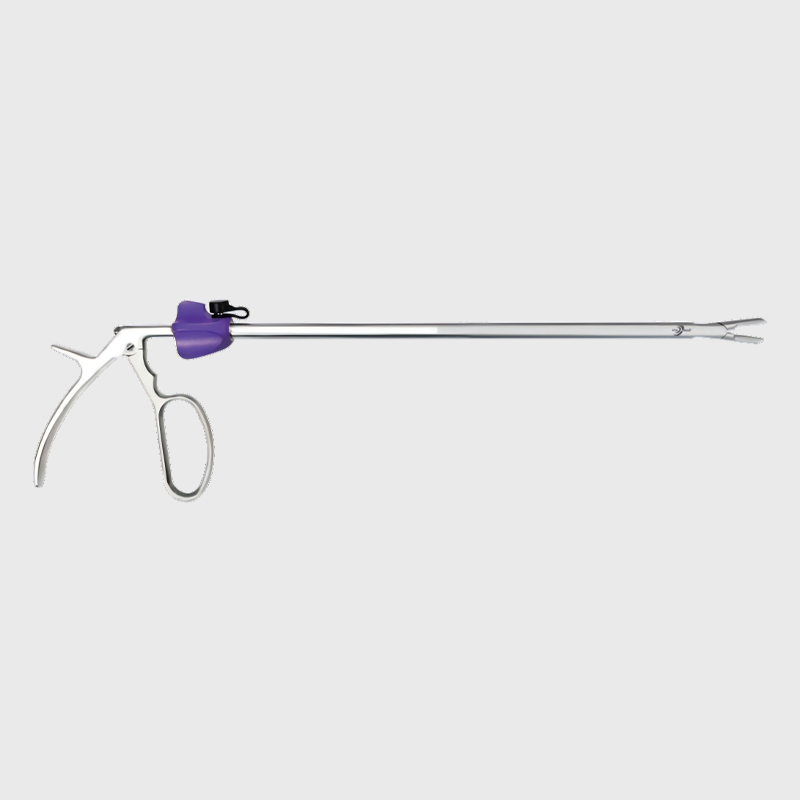
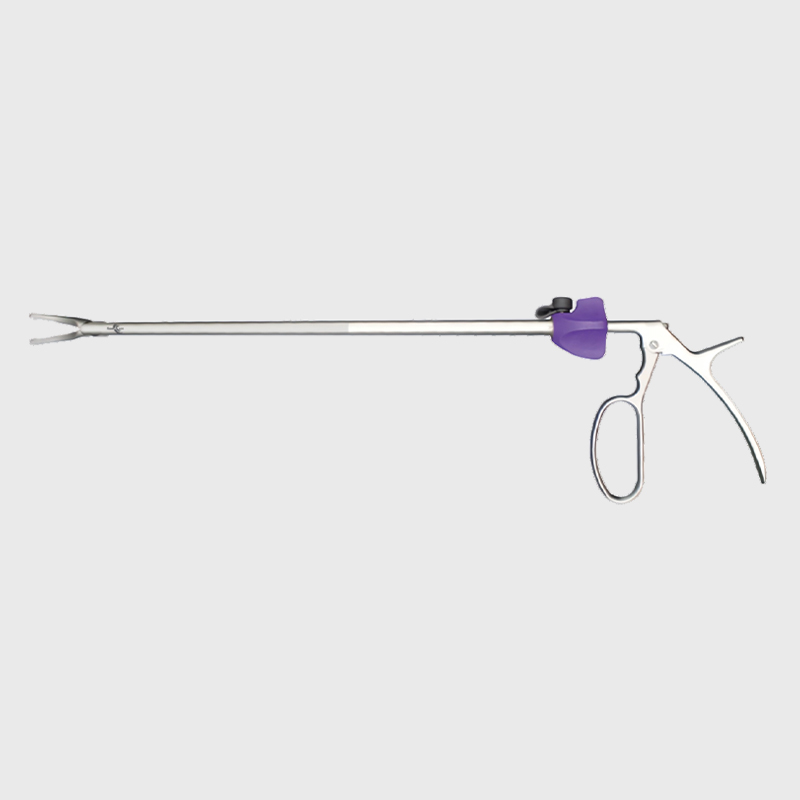
Surgical instruments, such as scissors, forceps, and needle holders, undergo rigorous cleaning and sterilization processes to ensure safety every time they are used. Trocars and laparoscopic staplers are crucial tools in minimally invasive surgery. The former is used to establish surgical access, while the latter enables efficient internal sutures, minimizing surgical trauma. Connecting systems, such as infusion lines and ventilator tubing, must ensure sterility and leak-tightness to prevent contamination from liquids or gases.
Laboratory equipment, such as culture dishes, centrifuge tubes, and pipettes, also require strict sterilization, especially in experiments like microbiological testing and cell culture. Laboratory disinfection and sterilization typically involves ultraviolet light, alcohol immersion, or high-pressure steam to ensure the accuracy of experimental results.



 English
English Español
Español Français
Français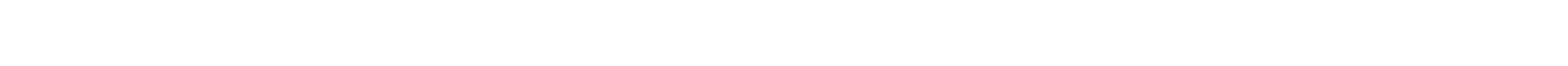



















 CONTACT US
CONTACT US